We have published a more recent review of this organization. See our most recent report on the SCI Foundation, formerly known as the Schistosomiasis Control Initiative.
More information:
Published: November 28, 2011
Summary
The Schistosomiasis Control Initiative (SCI) assists African governments with treatment of neglected tropical diseases and runs a number of smaller-scale projects (more).
SCI is a recommended organization because of its:
- Focus on a program with a strong track record and excellent cost-effectiveness (more).
- Demonstrated results - the research we have seen suggests that programs SCI has been involved with have been successful in reducing the prevalence of infection in the areas studied (more).
- Room for more funding - SCI has told us that it can use additional funding to expand its core programs and has committed to reporting on how additional funds are used and what results are achieved (more).
Our full review, below, discusses our full assessment of SCI, including what we see as its strengths and weaknesses as well as issues we have yet to resolve.
Our review process
We began reviewing SCI in 2009. Our review has consisted of:
- Reviewing published studies on SCI's programs.
- Extensive communications with SCI Director Alan Fenwick to discuss SCI's methods and funding needs, as well as meetings with other staff at SCI's headquarters in London.
- Requesting and reviewing SCI internal financial and organizational documents.
- Visiting a national schistosomiasis control program meeting and demonstration mass drug administration in Malawi (notes and photos from this visit)
Previous report on Schistosomiasis Control Initiative: April 2011 review.
Table of Contents
What do they do?
SCI works with governments in sub-Saharan Africa to create or scale up mass drug administration programs for neglected tropical diseases (NTD), particularly schistosomiasis and soil-transmitted helminths (STHs), in school-aged children and other groups determined to be at high risk.1 SCI's role has primarily been to solicit grants from large funders, identify country recipients, provide funding to governments for government-implemented programs, provide advisory support, and conduct research on the process and outcomes of the programs.
SCI does not report a comprehensive budget of all of its expenditures. It reports spending for each of its "accounts." It has accounts for each of the grants it has received, as well as an account for unrestricted donations. We have seen spending details for some of these accounts.
Large grants for mass drug administrations
SCI's work has been driven by a number of large grants, each with somewhat varied program designs and geographic coverage:
- Initial Gates Foundation grant: SCI was founded in 2002 through a $32 million grant from the Gates Foundation.2 This grant was used to create national treatment programs for schistosomiasis and soil-transmitted helminths (STHs) in six countries.3
- Grants for integrated NTD control: In 2006, SCI received large grants from USAID and the Gates Foundation to support integrated NTD programs in eight countries for five years to treat lymphatic filariasis, onchocerciasis, and trachoma, in addition to schistosomiasis and STHs.4 It received a grant in 2007 to expand its advisory work to Rwanda and Burundi.5 All of these grants were due to be completed in 2011.6
- DFID grant: In 2010, SCI received funding from the UK's Department for International Development for treating schistosomiasis and soil-transmitted helminths7 in eight countries over five years.8 Other NTDs are not covered by the grant, though DFID also provided funding to the Liverpool School of Tropical Medicine to integrate treatment for lymphatic filariasis with SCI-funded schistosomiasis and STH programs in six countries.9
SCI's role in mass drug administrations in general is to:10
- Advocate for the benefits of mass drug distributions to government officials.
- Assist with planning and fund raising.
- Deliver funding and drugs to governments.
- Provide financial management and technical support.
- Develop procedures for monitoring and evaluation.
Other projects
In addition, SCI has received some smaller grants and funding from individual donors. This funding has been used, or committed to be used in the future, for:
- Research. SCI has received a number of smaller grants to carry out research related to NTD control.11
- Small-scale NTD treatment programs. SCI told us that it has used donations from individuals to conduct small mass drug administration projects in Cote d'Ivoire (this country is now being funded with the DFID grant), Mozambique (through a doctor who works there), Uganda (on islands in Lake Victoria), and Burundi.12
- Other NTD-related activities. SCI has also used funding from individuals for surgeries for hydrocele (a symptom of lymphatic filariasis) in Niger, and health education and water and sanitation programs in Burundi.13
As of July 31, 2011, SCI had received about £361,000 (about $580,000) in donations from individuals (excluding a gift of £800,000 to support the national program in Burundi14 and including £150,000 in Gift Aid, i.e. tax benefits claimed from the UK government). Total spending in August 2009 to July 2011 is listed as £51,100, with an additional £221,000 in spending commitments and grants "about to be awarded."15 This source does not provide information on what funds have been spent on, but does list future projects. Planned spending included £66,000 for disease mapping and shipping costs for Cote d'Ivoire, £25,000 for hydrocoele treatments in Niger (SCI told us this will pay for 300 surgeries), £100,000 for Yemen (SCI told us this will pay for delivery of schistosomiasis treatments for 850,000 school-aged children; drugs are already available), and £50,000 for Senegal (SCI told us this will pay for delivery of treatments for 500,000 children; drugs are already available).16
Another source states that SCI had spent £112,179 of funds donated by individuals as of February 2011. This source lists each recipient organization or company, and includes £23,425 to a small group in Mozambique for deworming.17 We are unclear on what the purposes of the other expenses are.
Overall spending breakdown
We have seen a number of spending breakdowns from SCI, which vary in the amount of detail, the categories used, and the funding sources or years covered. We do not feel that any one source gives a comprehensive picture of how SCI has spent its money, so we present a few different breakdowns of SCI's expenditures:
- SCI provided a high-level breakdown of spending between its founding in 2002 and April 2010. In this period, SCI spent a total of $68.2 million, of which 59% was spent on country programs (we do not know what this includes), 28% on drugs, 9% on salaries, and 5% on "OHD/College contribution" (our understanding is that this is an administrative fee charged by the college that hosts SCI).18
- SCI also provided spending data for grants that were active as of April 2010 (the integrated NTD control grants discussed above). In aggregate, 48% of this funding had been transferred to governments,19 26% spent on "lab and works supplies," 12% spent on staff, 6% spent on overheads, and 8% spent on various other expenses.20
- For the one grant for which we have line-by-line transaction information, a Gates Foundation grant for Burkina Faso for 2006-2011, 70% was granted to the local NTD organization RISEAL and an additional 27% was spent on drugs and medical supplies.21
- As of January 2011 (the most recent report we have of SCI's full historical funding sources), SCI had received a total of $108 million over the course of its history, of which $42.6 million was from the Gates Foundation (39%), $16.7 million from the U.S. government through USAID (15%), and $38.3 million from the British government through DFID (35%).22 As discussed above, these grants have funded national treatment programs. As of July 2011 (the most recent report we have on donations from individuals), SCI had raised about £850,000 (about $1.31 million) from individuals.23
Does it work?
SCI's large-scale programs are focused on delivering treatments that have been both (a) independently studied in rigorous trials found to be effective, and (b) found to be effective in three national programs aided by SCI.
We have remaining concerns about whether the results found in SCI-aided programs are:
- representative of overall results in those countries. The studies only cover the first year or two of the program, and there are a number of ways in which the results may be biased (more
- representative of results in all SCI-aided countries (more)). We have only seen detailed results for three of the countries SCI has worked in.
- representative of results that would be achieved with donations from individuals. Donations from individuals may support smaller-scale programs, and we have not seen results from these programs (more).
We also have remaining questions about how many treatments are needed to have lasting impact, and how many treatments each individual receives in SCI's programs (more).
Independent evidence of program effectiveness
SCI's primary program is mass deworming, which we discuss extensively on another page. There is a very strong case that mass deworming is effective in reducing infections. The evidence on the connection to positive quality-of-life impacts is less clear, but there is a possibility that deworming is strongly beneficial.
Internal monitoring: large-scale programs
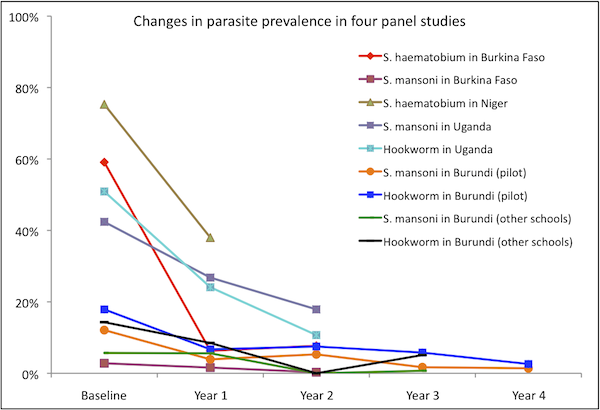
We have seen detailed technical reports for four countries: Burkina Faso, Niger, Uganda, and Burundi. The first three countries accounted for about 74% of SCI funding as of April 2010 (the most recent report we've seen that breaks down spending by country),24 though the data below covers only the first year or two of these programs, which started in 2003-2004 and have continued until at least 2010. We also include Burundi for which we have seen a technical report that appears to cover the full time period of SCI's work in the country. Burundi is the only country for which we have seen data on a program that was not funded by SCI's first Gates Foundation grant. Note that the data from Burundi is from two studies: (a) 2007-2011 results from schools included in a pilot program in three provinces; and (b) 2008, 2009, and 2011 results from schools in the other districts.
We focus on these countries because (a) these countries account for the bulk of SCI's spending and (b) we have the most in-depth information on them.
Results from Burkina Faso, Niger, Uganda, and Burundi
All of the following data is from uncontrolled panel studies, i.e. the same individuals were examined before and after treatment and the changes in their disease status reported as the effect of the treatment. Cross-sectional studies of children in the same schools as the cohort children and selected to match, in age and sex, the cohort group were also conducted in Burkina Faso with roughly similar results.25 In the four countries, significant decreases in parasite prevalence and intensity, anemia, and some disease manifestations were observed. All of the changes reported in the below table are statistically significant at p<0.05.26
| Schistosoma haematobium | Schistosoma mansoni | Hookworm | ||||
|---|---|---|---|---|---|---|
| Country | Changes in prevalence | Changes in intensity | Changes in prevalence | Changes in intensity | Changes in prevalence | Changes in intensity |
| Burkina Faso | 59.1% at baseline to 7.7% at two years | 94.2 eggs/10ml urine at baseline to 6.8 at two years | 2.8% at baseline to 0.3% at two years | 4.6 eggs per gram of feces at baseline to 0.6 at two years | Not reported | Not reported |
| Niger | 75.3% at baseline to 28% at one year | 22.8% prevalence of heavy-intensity infections at baseline to 4.6% at one year | Not reported | Not reported | Not reported | Not reported |
| Uganda | Not reported (SCI reports very low baseline prevalence27 ) | N/A | 42.4% at baseline to 17.9% at two years | 219.6 eggs per gram of feces at baseline to 37.4 at two years | 50.9% at baseline to 10.7% at two years | 309.4 eggs per gram of feces at baseline to 21.9 at two years |
| Burundi (pilot) | Not reported (SCI reports very low baseline prevalence28 ) | N/A | 12.7% at baseline to 1.7% at four years | Not reported | 17.8% at baseline to 2.7% at four years | Not reported |
| Burundi (other schools) | Not reported (SCI reports very low baseline prevalence29 ) | N/A | 6.2% at baseline to 0.7% at three years | Not reported | 15.1% at baseline to 5.4% at three years | Not reported |
For the other two prominent soil-transmitted helminths, ascaris and trichuris, very low prevalence of ascaris was reported in the Niger and Burkina Faso studies,30 and low baseline levels with modest decreases at two years were reported for both ascaris and trichuris in Uganda. In Burundi, effects on ascaris and trichuris appear inconsistent; prevalence both rose and fell by statistically significant amounts over the five years of the study (with the exception of trichuris, where the rise in prevalence was not statistically significant). Data from Uganda and Burundi are given in the footnote.31
| Country | Anemia | Mean hemoglobin concentration32 | Blood in urine33 | Ultrasound abnormalities of the urinary tract prevalence | Ultrasound abnormalities of the bladder | Thinness or wasting | Shortness or stunting | Firm or hard liver | Firm or hard spleen |
|---|---|---|---|---|---|---|---|---|---|
| Burkina Faso | 65.75% at baseline to 61.59% at one year | 10.97 g/dL at baseline to 11.25 g/dL at one year | Micro: 49.56% at baseline to 10.50% at one year | Not reported | Not reported | Not statistically significant | Not statistically significant | Not reported | Not reported |
| Niger | 61.9% at baseline to 50.4% at one year | 11.0 g/dL at baseline to 11.4 g/dL at one year | Gross: 7.1% at baseline to 0.4% at one year; Micro: 53.5% at baseline to 6.0% at one year | 45.6% at baseline to 15.2% at one year | 41.6% at baseline to 14.7% at one year | Not reported | Not reported | Not reported | Not reported |
| Uganda | 51.6% at baseline to 36.2% at two years | 11.4 g/dL at baseline to 12.0 g/dL at two years | Not reported | Not reported | Not reported | Not reported | Not reported | 63.3% at baseline to 0.8% at two years | 61.6% at basline to 14.1% at one year |
| Burundi (pilot) | 25.4% at baseline to 8.3% at four years | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Burundi (other schools) | 26.0% at baseline to 16.3% at three years | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
Potential issues with the above data
Due to the way in which they were carried out, these studies may overestimate SCI's impact. Potential sources of bias include:
- Monitoring of selected locations. It appears that the authors of the studies we've seen selectively chose locations to monitor, rather than examining a representative sample of treated areas.
- In Burkina Faso, monitoring occurred in four out of 13 regions that received treatment. These four regions were selected because they were "known a priori to be places where schistosomiasis is highly endemic."34
- In Niger, survey locations were stratified "to represent the two main transmission patterns in Niger," and all of the survey locations were located near bodies of water.35 SCI told us that these locations "are not representative of the treatment population as a whole. They were selected to indicate the impact of treatment in schools with varying prevalence and intensity of both [types of schistosomiasis]."36
- In Uganda, as in Niger, survey locations "were selected to represent different transmission settings."37 We have requested further information on how representative these transmission settings are of the treatment area as a whole, but have not yet received it."38
- In Burundi, pilot program "schools were chosen based on 3 zones; each containing different NTD endemicity": the "STHs + Schistosomiasis + onchocerciasis" zone, the "STHs +onchocerciasis" zone, and the "STH only endemic areas."39 For the survey of non-pilot program schools, the report we have seen says only, "The selection of schools was done randomly from the non-pilot provinces; taking into account 11 separate ecological zones."40
- Low follow up rates. Follow up rates tended to be quite low (43-73% over two years of study).41
SCI stated to us that the children that were available for follow up in most or all of the above studies were those children who had not dropped out of school and were not absent on the given day.42
There are a few ways in which this phenomenon could lead to overstatement of effectiveness:
- If schistosomiasis itself contributes to dropping out of school, then the children who are successfully followed up with may be the ones who are most likely to have ceased being infected for reasons unrelated to treatment.
- A similar dynamic could hold if a third factor (for example, low family income or poor hygiene) contributes to both schistosomiasis infection and dropping out of school.
- The children who are successfully found, year after year, seem (intuitively speaking) more likely to be the same children who are successfully treated, year after year. Therefore, effects of treatment on these children aren't necessarily representative of effects on the treated population as a whole.
The baseline characteristics measured in the studies did differ in some ways between those children who were found on follow up and those who were not; however the differences do not exhibit consistent patterns across the three studies (not reported for Burundi).43
- Possibility of unreported measured results. As seen in the above tables, many results are reported for one or two but not all of the countries. It is possible that some of these indicators were measured but not reported in the published studies because they did not show favorable results. This is a speculation only; we have not discussed this question with the studies' authors.
Do these results apply to SCI's large-scale programs generally?
We have limited information on whether the results presented above from Burkina Faso, Niger, Uganda, and Burundi can be generalized to other countries in which SCI has run programs (see footnote for details of where SCI has worked over what years and what results we have seen44 ). In addition to the published studies discussed above, we requested monitoring reports from Tanzania, which we did not receive.
For its first year or two of work in Mali and Tanzania, SCI posts results, but not details of how the data was collected, on its website. While reported results show positive effects, results are not reported for many indicators and we do not know if the methods used to collect this data were highly rigorous.45
SCI notes that in Zambia, which received support under SCI's initial Gates Foundation grant, implementation was poor and results below expectations.46
We have not seen evaluations of SCI's work on diseases other than schistosomiasis and soil-transmitted helminths and our understanding from conversations with SCI is that it does not monitor these programs. We have not seen evaluations of SCI's work with populations other than schoolchildren (note that adults may be targeted with unrestricted donations in the future – see below).
Internal monitoring: small-scale programs
We have seen limited information on the success of SCI's small-scale programs:
- We have seen a list of treatments given by community in Mozambique in 2008,47 and a narrative report that states, "Since 2006 surveying and treatment has taken place in 14 of the district’s primary schools, in which every child is administered with the correct dosage of Albendazole and Praziquantel annually."48
- For SCI's project in the Ugandan Islands of Lake Vicoria, we have seen an in-depth baseline report from 2009, but no follow up reports.49
- We have not seen any monitoring or evaluation from Cote d'Ivoire or the surgery program in Niger.
Possible negative and offsetting impact
- Concerns over whether treatment was sustained: We believe it is important that deworming programs are sustained over time, as re-infection is rapid and a one-time treatment may have little long-term effect.50
SCI told us that it "is hesitant to use one-off donations to fund programs that couldn't be continued over the long run,"51
and seems to have a reasonable record of maintaining national programs over time.52
However, it is not clear to us (a) how likely programs funded by individual donors are to be sustained after the first few years; (b) the extent to which SCI-funded programs have succeeded in treating the same children multiple times, as opposed to simply treating the same areas multiple times (and thus treating different children once each).
We remain unsure about how many treatments are needed to impact health. SCI told us that its views on what groups should be treated and how often "is largely based on intuition and common sense, though it usually works and SCI collects sufficient data to know when it isn't working. In general, in high endemicity areas re-infection is a major issue; in lower endemicity areas, a single treatment can be sufficient."53 One example of the variation in treatment patterns is what SCI told us about its program in Yemen:
SCI distinguishes between high, medium and low prevalence areas. In high prevalence areas, SCI treats the whole population once, and children for five years. In medium prevalence areas, SCI treats the whole population once, and children every other year. In low prevalence areas, SCI treats children every other year.54
- Replacement of government funding: In the past, SCI has largely supported programs that did not exist before its support.55 We have not seen data on government spending on NTDs before and after receiving SCI support.
- Diversion of skilled labor: Drug distribution occurs only once or twice per year and appears to be conducted by teachers, community drug distributors (who receive minimal training to fulfill this role), and health center staff.56 Given the limited time and skill demands of mass drug distribution,57 we are not highly concerned about distorted incentives for skilled professionals.
What do you get for your dollar?
The details of our calculation of SCI's full cost per treatment are in this spreadsheet. In short, using data on the value of SCI's grants from 2002-2010, the number of schistosomiasis and STH treatments it reports delivering during that period, and conversations with SCI about how the grants were used, we estimate:
- The upper-bound on the cost per treatment during this period was $0.79. This includes all grants received in "SCI's costs," with the exception of the DFID grant which was awarded in late 2010.
- Our best guess excludes a few more grants that, based on conversations with SCI, we believe can reasonably be excluded from the cost of treatment. This best guess is intended to be fairly conservative. Under these assumptions, we estimate the cost per treatment at $0.68.
- A less conservative estimate, that attempts to subtract out research costs that SCI told us were above and beyond normal monitoring and evaluation costs, yields $0.49 per treatment.
- A forward-looking estimate based on the funding received from DFID and the number of treatments committed under that grant, yields an expected cost of additional treatments of $0.51 (officially 3 treatments per 1 GBP), though (a) this does not include costs such as organizational overhead and (b) SCI notes that it is possible that this funding will be supplemented with other funding to achieve the treatment goals.
Note that SCI's USAID grants involved some treatments for diseases other than schistosomiasis and STHs; we do not include these on either side of the calculation, i.e., we do not include the treatments in the denominator of "cost per treatment" or the value of donated drugs in the numerator of "cost per treatment."
We discuss how the above figures relate to how much it costs to improve a child's health and development at our report on mass treatment programs for schistosomiasis and STHs.
Room for more funds?
SCI told us that how it would use additional unrestricted funding is dependent on the size of the donation received.
- Up to $50,000 it would hold this funding in a "response fund" for "unexpected and urgent projects." Examples of projects that might be funded from SCI's reserve fund include funding a doctor in Mozambique to deliver schistosomisis treatments in her area of work, extending treatment in some areas, SAFE washing kits for trachoma, and lymphatic filariasis leg washing kits, improved advocacy materials, and SCI staff attending conferences.58
- SCI would allocate the next $50,000 to disease mapping in Angola and Ethiopia, in order to prepare for potential national programs in those countries.59
- Above an additional $100,000 in unrestricted funding, it would use this money to supplement one of three large-scale programs:60
- Mozambique: Treating school children every year instead of every other year for schistosomiasis and helminths.
- Malawi: Treating pre-school children and at-risk adults for schistosomiasis and helminths.
- Senegal: Expanding treatment for schistosomiasis and helminths to schoolchildren in districts that are not currently receiving treatment or to adults, depending on disease mapping results and government preferences.
As of November 2011, SCI had committed to deliver, over five years, at least 90 million schistosomiasis and at least 100 million STH treatments to the eight countries funded by DFID.61 It also expects to deliver, with secured funding, 500,000 schistosomiais treatments per year and 4 million STH treatments every six months to Burundi, 200,000 schistosomiais and STH treatments per year to residents of Ugandan islands in Lake Victoria, and 30 million schistosomiasis and STH treatments to Yemen. As a one off programme, 500,000 children will be treated for schistosomiasis in Senegal in December 2012.62 If it receives additional funding over $100,000, we would expect the total number of treatments delivered to DFID-funded countries and Senegal to increase.
SCI told us that if it receives additional funding it will report what activities were funded, how many additional treatments for schistosomiasis and STHs were provided, what populations were treated, and methods and results of monitoring and evaluation.
In total, SCI estimates that it could use an additional $2 million each year for Mozambique, Malawi, and Senegal, starting in 2012, to treat an additional 4 to 6 million people.
Note that the proposed activities (listed above) for Mozambique, Malawi and Senegal are likely to be less beneficial than our discussion of deworming, taken in isolation, would imply. The evidence regarding deworming is generally based on bringing annual treatment to children who would not have been treated otherwise. The benefits of moving to annual treatment for children who were already going to receive every-other-year treatment - or of treating adults - are likely to be lower. In addition, the evidence regarding deworming is generally based on combination treatment for both schistosomiasis and soil-transmitted helminths, but Malawi and Senegal do not appear to have significant prevalence of soil-transmitted helminths (though Mozambique does).63
Financials
We discuss SCI's financials above.
Unresolved issues
While we believe that SCI is an outstanding organization, we list some unresolved issues below:
- As discussed in detail above, we have remaining concerns about SCI's evidence of effectiveness. While studies have implied success in reducing the prevalence of infection, we are concerned about how relevant the studied populations are to the full populations treated by the programs.
- Though we have researched the effect of schistosomiasis and STH infection on short- and long-term health, we lack confidence in the severity and frequency of symptoms. Based on the information we have seen, it seems that these infections cause little harm in most cases, but can cause moderate to severe long-term damage in a small percentage of cases.
- SCI's future funding priorities include activities whose likely impact is unclear to us, including treating adults and advocacy.
Sources
- Brooker, Simon et al. 2007. Cost and cost-effectiveness of nationwide school-based helminth control in Uganda: Intra-country variation and effects of scaling-up (PDF). Health Policy Plan 23(1): 24–35.
- Fenwick, Alan, et al. 2009. The Schistosomiasis Control Initiative (SCI): Rationale, development and implementation from 2002–2008. Parasitology 136: 1719-1730. Summary available at http://journals.cambridge.org/action/displayAbstract?fromPage=online&ai… (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/5sbwCb0Ht.
- Fenwick, Alan. SCI Director. Conversation with GiveWell, October 17, 2011.
- Fenwick, Alan. SCI Director. Email to GiveWell, February 1, 2011.
- Fenwick, Alan. SCI Director. Email to GiveWell, November 15, 2011.
- Fenwick, Alan. SCI Director. Email to GiveWell, November 17, 2011.
- Fenwick, Alan. SCI Director. Email to GiveWell, November 20, 2011.
- Fenwick, Alan. SCI Director. Phone conversation with GiveWell, July 2009.
- Fenwick, Alan. SCI Director. Phone conversation with GiveWell, June 17, 2010.
- Fenwick, Alan. SCI Director. Phone conversation with GiveWell, February 16, 2011.
- Fenwick, Alan. SCI Director. Phone conversation with GiveWell, September 15, 2011.
- Fenwick, Alan. SCI Director. Phone conversation with GiveWell, November 15, 2011.
- Fenwick, Alan. SCI Director. Phone conversation with GiveWell, November 28, 2011.
- Gabrielli, Albis-Francesco et al. 2006. A combined school- and community-based campaign targeting all school-age children of Burkina Faso against schistosomiasis and soil-transmitted helminthiasis: Performance, financial costs and implications for sustainability. Acta Tropica 99(2-3): 234-242. Abstract available at http://www.sciencedirect.com/science/article/pii/S0001706X06001471 (accessed November 4, 2011).
- Gates Foundation. Imperial College London (June 2002). http://www.gatesfoundation.org/Grants-2002/Pages/Imperial-College-Londo… (accessed November 3, 2011). Archived by WebCite® at http://www.webcitation.org/62vg8K7vD.
- GiveWell. Email to Narcis Kabatereine (DOC), September 27, 2011.
- GiveWell. Interpreting the disability-adjusted life-year (DALY) metric.
- GiveWell. Mass drug administration to control onchocerciasis.
- GiveWell. Mass drug administration to control schistosomiasis and soil-transmitted helminths.
- GiveWell. Mass drug administration to eliminate lymphatic filariasis.
- GiveWell. SAFE strategy to control trachoma.
- Global Atlas of Helminth Infections. Malawi. http://www.thiswormyworld.org/maps/malawi (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/63Ytiow9S
- Global Atlas of Helminth Infections. Mozambique. http://www.thiswormyworld.org/maps/mozambique (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/63Ytj3Kwb
- Global Atlas of Helminth Infections. Senegal. http://www.thiswormyworld.org/maps/senegal (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/63Ytj6S7D.
- Kabatereine, Narcis B., et al. 2006. The control of schistosomiasis and soil-transmitted helminths in East Africa. Trends in Parasitology 22(7): 332-339. Abstract available at http://www.sciencedirect.com/science/article/pii/S1471492206001048.
- Kabatereine, Narcis B., et al. 2007. Impact of a national helminth control programme on infection and morbidity in Ugandan schoolchildren. Bulletin of the World Health Organization 85: 91-99.
- Koukounari, Artemis et al. 2007. Schistosoma haematobium infection and morbidity before and after large-scale administration of praziquantel in Burkina Faso (PDF). Journal of Infectious Diseases 196:659–69.
- MANNA. A firsthand look at the problems and pathways to controlling schistosomiasis in Mozambique (DOC).
- MANNA. Campanha do controle de shistosomiase e parasitoses intestinais (February to June 2008) (XLS).
- Miguel, Edward and Michael Kremer. 2004. Worms: Identifying impacts on education and health in the presence of treatment externalities (PDF).
- Phillips, Anna. SCI Country Program Manager for Burkina Faso and Niger. Email to GiveWell (DOC), October 13, 2011.
- RISEAL. Homepage. http://www.riseal.org/index2.html (accessed November 3, 2011). Archived by WebCite® at http://www.webcitation.org/62vgrHOCC.
- Schistosomiasis Control Initiative. Account summary (May 2011) (JPEG).
- Schistosomiasis Control Initiative. Board management accounts (April 2010) (PDF).
- Schistosomiasis Control Initiative. Burkina Faso: Impact. http://www3.imperial.ac.uk/schisto/wherewework/burkinafaso/burkinafasoi… (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/5sc48n1yv.
- Schistosomiasis Control Initiative. Burundi: Impact. http://www3.imperial.ac.uk/schisto/wherewework/burundi/burundiimpact (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/5scR0RjN3.
- Schistosomiasis Control Initiative. Burundi: Strategy. http://www3.imperial.ac.uk/schisto/wherewework/burundi/burundistrategy (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/5scPivJhr.
- Schistosomiasis Control Initiative. Expenditures list (November 2006-February 2011).
- Schistosomiasis Control Initiative. Funding of programmes with donations from individuals.
- Schistosomiasis Control Initiative. Gates Foundation final report (January 2011) (DOC).
- Schistosomiasis Control Initiative. Gates2 Burkina Faso spending report (PDF).
- Schistosomiasis Control Initiative. Gates2 Y1 to Y5 accounts (PDF).
- Schistosomiasis Control Initiative. Grants for 2012 (November 2011) (XLS).
- Schistosomiasis Control Initiative. IC Trust summary (September 2011) (XLS).
- Schistosomiasis Control Initiative. ICOSA 6-year PZQ forecast.
- Schistosomiasis Control Initiative. Imperial initiative to protect children from tropical disease awarded £25m government backing. http://www3.imperial.ac.uk/newsandeventspggrp/imperialcollege/newssumma… (accessed November 3, 2011). Archived by WebCite® at http://www.webcitation.org/63nqmTE5d.
- Schistosomiasis Control Initiative. Mali: Impact. http://www3.imperial.ac.uk/schisto/wherewework/mali/maliimpact (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/5scPHop3a.
- Schistosomiasis Control Initiative. Monitoring and evaluation report for Burundi (DOC).
- Schistosomiasis Control Initiative. Neglected tropical diseases in Mozambique. SCI asked that we keep this document confidential.
- Schistosomiasis Control Initiative. Niger: Impact. http://www3.imperial.ac.uk/schisto/wherewework/niger/nigerimpact (accessed September 16, 2010. Archived by WebCite® at http://www.webcitation.org/5smNthzdi.
- Schistosomiasis Control Initiative. Proposal by SCI, Imperial College to manage the Program for Integrated Control of Neglected Tropical Diseases in Côte d'Ivoire. SCI asked that we keep this document confidential.
- Schistosomiasis Control Initiative. Rwanda: Impact. http://www3.imperial.ac.uk/schisto/wherewework/rwanda/rwandaimpact (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/5scQwHDti.
- Schistosomiasis Control Initiative. Rwanda: Strategy. http://www3.imperial.ac.uk/schisto/wherewework/rwanda/rwandastrategy (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/5scPnJJIY.
- Schistosomiasis Control Initiative. Schistosomiasis, soil transmitted helminths and malaria survey/control in Lake Victoria islands in Uganda (DOC).
- Schistosomiasis Control Initiative. Strategic plan (2010-2015) (DOC).
- Schistosomiasis Control Initiative. Summary sheet of treatments instigated and overseen by SCI (XLS).
- Schistosomiasis Control Initiative. Tanzania: Impact. http://www3.imperial.ac.uk/schisto/wherewework/tanzania/tanzaniaimpact (accessed September 9, 2010). Archived by WebCite® at http://www.webcitation.org/5sbwJEGqB.
- Schistosomiasis Control Initiative. USAID RTI Y1 to Y3 accounts. SCI asked that we keep this document confidential.
- Schistosomiasis Control Initiative. What we do. http://www3.imperial.ac.uk/schisto/whatwedo (accessed September 10, 2010). Archived by WebCite® at http://www.webcitation.org/5sdLNO10H.
- Styles, Benjamin. SCI Senior Biostatistician. Phone conversation with GiveWell, August 12, 2011.
- Tohon, Zilahatou B., et al. 2008. Controlling schistosomiasis: Significant decrease of anaemia prevalence one year after a single dose of praziquantel in Nigerien schoolchildren (PDF). PLoS Negl Trop Dis 2: e241.
- Touré, Seydou, et al. 2008. Two-year impact of single praziquantel treatment on infection in the national control programme on schistosomiasis in Burkina Faso (PDF). Bulletin of the World Health Organization 86: 780–787.
- Weldon, Alexandra. SCI Advocacy and Relations Officer. Phone conversation with GiveWell, August 5, 2011.
- 1
"Objectives of SCI
- To encourage development of sustainable schistosomiasis and STH control programmes in sub-Saharan Africa.
- In the selected countries: to reach at least 75% of school-aged children (which in most countries would be from 6 to 15-year-old) and other high-risk groups with chemotherapy, namely PZQ and ALB; and thereby reducing prevalence and intensity of schistosomiasis and STH infections; as well as reducing schistosomiasis-related morbidity in high risk groups; and burdens due to STH infections in the targeted populations.
- To create a demand for sustained schistosomiasis and STH control.
- To promote access to anthelminthic drugs and good case management in the regular health system.
- To develop a rigorous monitoring and evaluation plan which will generate the information required to determine whether or not the objectives have been met."
Fenwick et al. 2009, Pg 3.
- 2
"The move towards national control programmes in sub-Saharan Africa was facilitated by an award from the Bill and Melinda Gates Foundation (BMGF; http://www.gatesfoundation.org) Global Health Program in 2002, to the SCI for the implementation and evaluation of control of schistosomiasis." Fenwick et al. 2009, Pg 2.
Amount at Gates Foundation, "Imperial College London (June 2002)." - 3
"Six countries were selected by October 2003 for full support: Burkina Faso, Mali, Niger, Uganda, Tanzania and Zambia. The countries each proposed a different implementation approach and management structure for their large-scale schistosomiasis control. This was readily accepted because the BMGF required SCI to test the ‘proof-of-principle’ of national scale, Ministry of Health (MoH)-led schistosomiasis control programmes. SCI is based in Imperial College London and operated with the principle that all programmes were country owned and run, with SCI staff offering technical and other assistance, but not as expatriates living in-country. Programmes were based in the MoH in the respective country, and SCI offered support to improve the national health system." Fenwick et al. 2009, Pg 2.
Between 2003 and 2008, SCI provided treatment for schistosomiasis and soil-transmitted helminths to the following number of people (Fenwick, et al. 2009, Pg 3, Table 1).
Number treated by country (millions) Year Uganda Burkina Faso Niger Mali Tanzania Zambia 2003 0.43 - - - 0.10 - 2004 1.23 1.03 0.67 - 0.44 - 2005 2.99 2.30 2.01 2.60 2.95 - 2006 1.51 2.82 1.56 2.18 0.38 0.56 2007 1.81 0.75 2.07 0.65 2.65 0.25 2008 1.50 2.70 5.28 - 1.24 - - 4
"Current and future rounds of treatment in all six countries are being delivered in an integrated manner to include schistosomiasis, STH, lymphatic filariasis, onchocerciasis and trachoma." Fenwick et al. 2009, Pg 10. The "six countries" refers to the six countries funded by SCI's first Gates Foundation grant.
Countries and dates from Schistosomiasis Control Initiative, "Board Management Accounts (April 2010)." - 5
Schistosomiasis Control Initiative, "Burundi: Strategy."
Schistosomiasis Control Initiative, "Rwanda: Strategy."
Schistosomiasis Control Initiative, "Board Management Accounts (April 2010)." - 6
Schistosomiasis Control Initiative, "Account Summary (May 2011)."
- 7
"A team from Imperial College London has been awarded 25 million funding from the UK Government to continue its fight against neglected tropical diseases, it was announced this week. The money will enable the Schistosomiasis Control Initiative (SCI) to provide 75 million treatments to protect some of the world’s poorest children against schistosomiasis – an illness caused by parasitic worms – and soil-transmitted helminths (STH). £15 million of the funding will be spent directly on procuring drug treatments, through an organisation called Crown Agents. The rest will be administered by SCI." Schistosomiasis Control Initiative, "Imperial Initiative to Protect Children from Tropical Disease Awarded £25m Government Backing."
- 8
Alan Fenwick, conversation with GiveWell, October 17, 2011.
- 9
"SCI will be assisted in their drug delivery by the Centre for Neglected Tropical Diseases at Liverpool School of Tropical Medicine via a sub contract through LATH (Liverpool Associates in Tropical Health). In six countries, this will lead to treatment for lymphatic filariasis – another worm disease – becoming integrated with schistosomiasis and STH treatment." Schistosomiasis Control Initiative, "Imperial Initiative to Protect Children from Tropical Disease Awarded £25m Government Backing."
- 10
- Alan Fenwick, phone conversation with GiveWell, June 17, 2010.
- Schistosomiasis Control Initiative, "Summary Sheet of Treatments Instigated and Overseen by SCI."
- Schistosomiasis Control Initiative, "Proposal by SCI, Imperial College to Manage the Program for Integrated Control of Neglected Tropical Diseases in Côte d'Ivoire."
- 11
SCI's summary of active accounts as of May 2011 lists five research grants totaling £1.9 million, or about $3 million. Schistosomiasis Control Initiative, "Account Summary (May 2011)."
- 12
"For the smaller donor, we have two or three projects, which we have been supporting and which will hopefully lead to pilot project in their respective countries.
- In Cote d'Ivore, we now have funding from the U.K. Department for International Development (DFID). There will eventually be a national program.
- In Mozambique, we have a doctor running a practice for 70,000 people. We have been funding her to test people, do surveys and give drugs to treat people. Up until now, that has taken all the individual funding that comes in.
Once we have people that want to give at least $100,000, we talk to them directly. Two examples:
- Someone wanted to do something special with his money, so we're doing hydrocele surgery in Niger. He gave us $200,000 and we told him we could do ~1000 hydrocele surgeries.
- Another person was interested in Uganda. So, we identified islands there in Lake Victoria that are relatively accessible and provided treatments there."
Alan Fenwick, phone conversation with GiveWell, February 16, 2011.
Funds committed for future use listed in Schistosomiasis Control Initiative, "IC Trust Summary (September 2011)":- Disease prevalence mapping in Cote D'Ivoire (£16,000)
- Shipping donated drugs to Cote D'Ivoire (£50,000)
- Burundi (£640,000). SCI told us that this was being used to continue an mass drug administration program that ran out of funds. Alan Fenwick, conversation with GiveWell, September 15, 2011.
- Unspecified activities in Yemen (£100,000) and Senegal (£30,000)
- Hydrocoele treatments in Niger (£25,000)
- 13
Alan Fenwick, conversation with GiveWell, September 15, 2011. Note: "SCI generally doesn't do water and sanitation programs because of the expense. In Burundi they're doing water and sanitation programming because they have been successful there with running a program and treating schistosomiasis, but soil-transmitted helminth infections remain persistent." Alan Fenwick, conversation with GiveWell, October 17, 2011.
- 14
Schistosomiasis Control Initiative, "IC Trust Summary (September 2011)" shows £640,000 allocated to Burundi. SCI told us that an additional £160,000 of Gift Aid funds (tax benefits claimed from the UK government) are also committed to Burundi. Alan Fenwick, email to GiveWell, November 17, 2011.
- 15
The month-by-month report on "IC Trust" we've seen covers the period August 2009 to July 2011 and shows a total of £51,100 spent. It does not specify what this was spent on. Schistosomiasis Control Initiative, "IC Trust Summary (September 2011)."
- 16
Schistosomiasis Control Initiative, "IC Trust Summary (September 2011)."
Further detail from Alan Fenwick, email to GiveWell, November 17, 2011.
Note that the first source says that £30,000 had been committed for Senegal and the second indicates that this amount had risen to £50,000. - 17
Schistosomiasis Control Initiative, "Expenditures List (November 2006-February 2011)." These are listed as "MANNA."
- 18
Schistosomiasis Control Initiative, "Board Management Accounts (April 2010)."
"When SCI claims back from USAID, a small % -- about 6% -- is an overhead charge that goes to Imperial College. SCI is not a registered charity but a part of Imperial College." Alan Fenwick, phone conversation with GiveWell, February 16, 2011. - 19
The line item is "external consultants." SCI told us, "The line 'external consultants' which seems a high personnel cost in some sub awards is in fact a transfer to the Countries - which for the sake of Imperial accounting are classed as 'external consultants' because Imperial College accounting system has no line for field work in Africa." Alan Fenwick, email to GiveWell, February 1, 2011.
- 20
Schistosomiasis Control Initiative, "Board Management Accounts (April 2010)."
Note that a source covering slightly different dates and grants reported a slightly different breakdown. Aggregating spending data from the Gates Foundation (2006-2011) and USAID (2006-2009) integrated control grants, we estimate that SCI spent about 38% of this funding on "field work expenses," 25% on drugs, 21% on staff, and 17% on various other expenses. We are unclear what "field work expenses" signifies. For the one country for which we have more detail, Burkina Faso, "field work expenses" were grants to the organization RISEAL, which is described on its website as "a federation of associations operating in West Africa, Madagascar, and in Europe" to "promote the control of Neglected Tropical Diseases" (RISEAL, "Homepage."). However, it is our understanding from conversations with SCI that much of its funding is often channelled via governments. Data from Schistosomiasis Control Initiative, "Gates2 Y1 to Y5 Accounts" and Schistosomiasis Control Initiative, "USAID RTI Y1 to Y3 Accounts." - 21
Schistosomiasis Control Intiative, "Gates2 Burkina Faso Spending Report."
- 22
Schistosomiasis Control Initiative, "Gates Foundation Final Report (January 2011)," Pg 20.
- 23
Schistosomiasis Control Initiative, "IC Trust Summary (September 2011)."
- 24
Data on spending by country is from Schistosomiasis Control Initiative, "Board Management Accounts (April 2010)," Pg 1. Funding, as of April 2010, was concentrated in Burkina Faso (34% of country-specific funding), Niger (33%), Uganda (10%), Burundi and Rwanda (10%; we don't have data for these countries independently), and Tanzania (7%).
- 25
"In addition to the cohort follow-up, a cross-sectional survey was conducted during the second follow-up (2 years post-treatment), in which a group of children (7–14 years old) outside the original cohort were randomly selected and examined in the sentinel schools. The number, age and sex structures were matched to those in the cohort who were present at the second follow-up in each school. Infection status in these children should represent the quality of treatment in children outside cohorts in schools, to confirm and validate the cohort data, i.e. no preferred treatment was given to cohort children…As in the cohort data, the proportion of heavy [S. haematobium infections was reduced from 25% to just 3.2% (Fig. 2). However, these children outside the cohort did show a slightly higher prevalence and intensity of S. haematobium infection than those in the cohort as in Table 1 (P<0.01) at 2 years post-treatment…In baseline children (7–14 years old) in the original cohort in this region, prevalence of S. mansoni infection was 14.2% (95% CI: 10.8–17.6; n = 408) [13.6% in the cohort baseline] and intensity of infection was 23.0 epg (95% CI: 11.8–34.2; n = 408) [22.4 epg in cohort] before treatment. Two years after treatment, S. mansoni prevalence in this region was 7.6% (95% CI: 4.4–11.0; n = 248) [1.5%in cohort] and intensity of infection was 16.5 epg (95% CI: 1.9–31.0; n = 248) [2.9 epg in cohort] (both P>0.05)." Touré et al. 2008, Pg 781-783.
- 26
Sources for the data in the tables:
- Burkina Faso: Touré et al. 2008 and Koukounari et al. 2007.
- Niger: Tohon et al. 2008.
- Uganda: Kabatereine et al. 2007.
- Burundi: Schistosomiasis Control Initiative, "Monitoring and Evaluation Report for Burundi."
- 27"S. haematobium occurs only in a small focus and is of minor public health significance." Kabatereine et al. 2007, Pg 91.
- 28Alan Fenwick, phone conversation with GiveWell, November 28, 2011.
- 29Alan Fenwick, phone conversation with GiveWell, November 28, 2011.
- 30
- "Very low prevalence (0.3 to 0.7%) of Ascaris lumbricoides infection was observed in 5 schools, while 3% of the schoolchildren were infected in 1 school (Sanguile) and no infection was observed in 2 schools (Kaou and Tabalak)." Tohon et al. 2008, Pg 3.
- "For both years examined, Ascaris lumbricoides infection was absent, and the prevalence of Trichuris trichura infection was estimated to be 1.1% at baseline and totally absent 1 year later." Koukounari et al. 2007, Pg 663.
- 31
Results from Kabatereine et al 2007, Pg 93, Table 2 (see source for 95% confidence intervals) and Schistosomiasis Control Initiative, "Monitoring and Evaluation Report for Burundi" (see source for statistical significance). We report "as measured results" for Burundi; SCI also reports model results.
Baseline Year 1 Year 2 Year 3 Year 4 Ascaris in Uganda 2.8% 1.6% 0.6% - - Trichuris in Uganda 2.2% 2.5% 1.6% - - Ascaris in Burundi (pilot) 14.9% 12.9% 20.1% 10.6% 10.1% Trichuris in Burundi (pilot) 3.2% 1.8% 3.9% 1.5% 2.4% Ascaris in Burundi (other schools) 21.6% 11.7% - 9.1% - Trichuris in Burundi (other schools) 10.4% 10.0% - 4.3% - - 32Hemoglobin is a component of blood containing iron. Anemia is defined as a hemoglobin concentrations below an age-dependent threshold.
- 33Gross haematuria: visible blood in the urine; Micro-haematuria: blood in the urine that is detectable by microscopic inspection.
- 34
"The SCI-supported schistosomiasis control program was implemented during 2004 and had treated 3,322,564 school-aged children in the 13 regions of the country through October 2006...For the present study, parasitological and morbidity data were collected from a cohort of 1727 Burkinabé children 6–14 years old, randomly sampled from 16 schools before and 1 year after chemotherapy (2004 and 2005, respectively). The schools included in these surveys were randomly selected from all schools in 4 Regional Health Directorates known a priori to be places where schistosomiasis is highly endemic." Koukounari et al. 2007. Pg 660.
- 35
"Eight villages located in schistosomiasis endemic regions were randomly selected to represent the two main transmission patterns in Niger: six villages located near permanent (Tabalak, Kokorou) or semi-permanent (Kaou, Mozague, Rouafi, and Sabon Birni) ponds and two (Saga Fondo, Sanguile) located along the Niger River. The villages represented the south-western region (Tillabe´ry) and the central-northern region (Tahoua) of the country, with four villages from each region. One village is located in the Sudanian climatic zone and the seven others are in the Sahelian climatic zone." Tohon et al. 2008, Pg 2.
- 36
Anna Phillips, email to GiveWell, October 13, 2011.
- 37
Kabatereine et al. 2007, Pg 92.
- 38
GiveWell, email to Narcis Kabatereine, September 27, 2011.
- 39
Schistosomiasis Control Initiative, "Monitoring and Evaluation Report for Burundi," Pg 1.
- 40
Schistosomiasis Control Initiative, "Monitoring and Evaluation Report for Burundi," Pg 13.
- 41
- Uganda: "We enrolled 4351 children from 37 schools, of which 2815 (64.7%) were traced and treated at one year follow-up and 1871 (43.0%) at two year follow-up." Kabatereine et al. 2007, Pgs 93-94.
- Burkina Faso: "Of 1727 schoolchildren recruited at baseline, 763 were successfully traced and re-examined at both follow-ups with three complete sets of longitudinal parasitological data on S. haematobium... Among 763 children, 322 had valid data entry for S. mansoni at all three surveys." Touré et al. 2008, Pgs 781-782.
- Niger: "Of the 1656 children recruited at baseline, 1193 (72.04%) were successfully followed-up in both year 1 and year 2 surveys." Schistosomiasis Control Initiative, "Niger: Impact."
- Burundi: In the pilot program survey, 53.3% of children surveyed at baseline were found for disease prevalence testing at the fourth follow up; however, only 49.6% were found at the first follow up, indicating that not all children found at the fourth follow up were found in all four follow ups. 64.8% were found for anemia testing at the fourth follow up (but only 60.5% at the first follow up). In the other schools survey, 56.5% of children surveyed at baseline were found for disease prevalence testing at the second follow up. 56.7% were found for anemia testing at the fourth follow up. Schistosomiasis Control Initiative, "Monitoring and Evaluation Report for Burundi," Pgs 1 and 13.
- 42
Benjamin Styles, phone conversation with GiveWell, August 12, 2011.
- 43
- Burkina Faso: "Baseline characteristics of children successfully followed-up showed that they had a lower mean age (9.6 years versus 11.0 years; P<0.01), a lower proportion of boys (54.1% versus 59.1%; P<0.05), higher S. haematobium prevalence (59.9% versus 53.1%; P$lt;0.01) but a similar intensity of S. haematobium infection (93.3 e/10 ml versus 91.2 e/10 ml; P<0.05), compared with those who had dropped out." Touré et al. 2008, Pgs 781-782.
- Niger: "Compared to those children who remained in the study cohort, the 216 children who dropped out after the initial survey differed significantly in the prevalence of S. haematobium infection (75.4% vs. 78%, respectively), but had less frequently heavy-intensity infections (22.8% vs. 16.5%, respectively). On the other hand, they did not differ in mean age (8.7 vs. 8.9 years, respectively), in the prevalence of anaemia (61.9% vs. 59.7%, respectively) nor in mean haemoglobinemia (11.04 g/dl vs. 11.03 g/dl, respectively)." Tohon et al. 2008, Pg e241.
- Uganda: "The baseline characteristics did not differ significantly among those included in the evaluation one-year post treatment and those lost to follow-up (see Table 1, available at http://www.who.int). However, we found the prevalence and mean intensity of S. mansoni to be significantly higher among those children who were lost to follow-up compared to those successfully followed up two years post treatment." Kabatereine et al. 2007, Pgs 93-94.
- 44
Funding sources in table below are compiled from:
Schistosomiasis Control Initiative, "Summary Sheet of Treatments Instigated and Overseen by SCI."
Alan Fenwick, phone conversation with GiveWell, June 17, 2010.
Schistosomiasis Control Initiative, "Board Management Accounts (April 2010)."
Funding for mass treatment | Have we seen disease prevalence/intensity or morbidity results? 2003 2004 2005 2006 2007 2008 2009 2010 2011 Burkina Faso - Gates | Results with details Gates | Results with details Gates/ USAID | Results with details Gates/ USAID | Results without details Gates/ USAID | No results Gates / USAID | No results Gates / USAID | No results ? Burundi - - - - GNNTDC | Results with details GNNTDC | Results with details GNNTDC | Results with details GNNTDC | Results with details Individual | Results with details Cote D'Ivoire - - - - - - - - DFID | No results yet Liberia - - - - - - - - DFID | No results yet Malawi - - - - - - - - DFID | No results yet Mali - Gates | Results without details Gates | Results without details Gates/ USAID | Results without details USAID | No results USAID | No results USAID | No results (Taken over by HKI) (Taken over by HKI) Mozambique - - - - - - - - DFID | No results yet Niger - Gates | Results with details Gates | Results with details Gates/ USAID | Results without details Gates/ USAID | No results Gates/ USAID | No results Gates/ USAID | No results Gates/ USAID | No results DFID | No results yet Rwanda - - - - GNNTDC | No results GNNTDC | No results GNNTDC | No results GNNTDC | No results ? Tanzania Gates | Results without details Gates | Results without details Gates | No results Gates | No results Gates | No results Gates | No results Gates | No results Gates | No results DFID | No results yet Uganda Gates | Results with details Gates | Results with details Gates | Results with details Gates/ USAID | Results without details Gates/ USAID | No results Gates/ USAID | No results Gates/ USAID | No results Gates/ USAID | No results DFID | No results yet Yemen - - - - - - World Bank | No results World Bank | No results World Bank | No results yet Zambia - Gates | Known failure Gates | Known failure Gates | Known failure Gates | Known failure - - - DFID | No results yet - 45
Schistosomiasis Control Initiative, "Mali: Impact."
Schistosomiasis Control Initiative, "Tanzania: Impact."Schistosoma haematobium Schistosoma mansoni Hookworm Anemia Country Follow up rate Changes in prevalence Changes in intensity Changes in prevalence Changes in intensity Changes in prevalence Changes in intensity Changes in prevalence Changes in mean haemoglobinemia Mali 58% over two years About 90% at baseline to about 50% at two years About 30% prevalence of heavy-intensity infections at baseline to about 3% at one year About 21% at baseline to about 13% at two years Not reported About 7% at baseline to about 2% at two years Not reported Not reported Not reported Tanzania 65% at one year Not reported Not reported in aggregate; about 3-52% at basline to 2-10% at follow up Not reported Not reported 39.81% at baseline to about 17.36% at one year Not reported 47.15% at baseline to about 32.97% at one year Not reported - 46
"Zambia has been less successful in reaching its original programme target of expanding coverage to treating 2 million school-aged individuals and had only achieved, according to incompletely reported coverage, around 25% of this target by July 2007." Fenwick et al. 2009, Pg 9.
- 47
MANNA, "Campanha do Controle de Shistosomiase e Parasitoses Intestinais (February to June 2008)."
- 48
MANNA, "A Firsthand Look at the Problems and Pathways to Controlling Schistosomiasis in Mozambique."
- 49
Schistosomiasis Control Initiative, " Schistosomiasis, Soil Transmitted Helminths and Malaria survey/Control in Lake Victoria Islands in Uganda."
- 50
"Single-dose oral therapies can kill the worms, reducing ... infections by 99 percent ... Reinfection is rapid, however, with worm burden often returning to eighty percent or more of its original level within a year ... and hence geohelminth drugs must be taken every six months and schistosomiasis drugs must be taken annually." Miguel and Kremer 2004, Pg 161.
- 51
Alan Fenwick, conversation with GiveWell, October 17, 2011.
- 52
See table "Funding for mass treatment | Have we seen disease prevalence/intensity or morbidity results?" in previous footnote.
- 53
Alan Fenwick, conversation with GiveWell, October 17, 2011.
- 54
Alan Fenwick, conversation with GiveWell, October 17, 2011.
- 55
- Uganda: "The first country to implement a control programme on a national scale...Uganda implemented the SCI-supported control programme in April 2003." Kabatereine 2007, Pg 91.
- Burkina Faso: "Some small-scale control activities with treatment had taken place in some areas in the past,11,13 but the national control programme did not start until 2004." Touré et al. 2008, Pg 780.
- Niger: "Niger’s National Schistosomiasis and Soil-Transmitted Control Programme (PNLBG) was launched at 2004." Fenwick et al. 2009, Pg 5.
- Mali: "In the following years many planned activities were not implemented due to limited financial resources but finally in 2004 national control activities recommenced in the country with support from the SCI." Fenwick et al. 2009, Pg 5.
- Tanzania: "The failure to embrace a national treatment programme has been due primarily to the costs involved in reaching the millions of individuals estimated to be at risk of infection, and the Ministry of Health was never able to support treatment within their budget. In October 2003, the Tanzanian National Plan was approved for funding by the SCI as a step towards developing a sustainable control programme." Kabatereine et al. 2006, Pg 334.
- Zambia: "'The Zambian Bilharzia Control Programme' (ZBCP) was established in 2004 to develop a MoH and MoE joint strategy for bilharzia and worm control. The MoE was already in receipt of a grant from the United States Agency for Inter- national Development (USAID) for implementing training and treatment in some schools on a small scale in two provinces, Eastern and Southern, which was known as the ‘School Health and Nutrition programme’ (SHN)." Fenwick et al. 2009, Pg 4.
- 56
"Drug distribution channels:
- School-based delivery for school children. School teachers will be trained to carry out drug distribution at schools.
- Community-based delivery for school-aged children who are not attending school and for community adults at high risk. Community Drug Distributors (CDD) will be trained to deliver the drugs at community.
- Health centre-based delivery. Drugs will be made available at health centres for those in the community who do not qualify for MDA and who request for treatment. Health workers at the centres will be trained.
Drug distributors need a minimum of one day’s training to understand the basis for calculating dosages, the necessary actions to deal with side-effects and treatment record keeping and reporting." Schistosomiasis Control Initiative, "Neglected Tropical Diseases in Mozambique," Pg 23.
"For schistosomiasis and STHs, treatment will be conducted through schools by the teachers. For LF, treatment will be conducted through community directed treatment, by the CDDs and community health agents, managed by the district medical officer." Schistosomiasis Control Initiative, "Proposal by SCI, Imperial College to Manage the Program for Integrated Control of Neglected Tropical Diseases in Côte d'Ivoire," Pg 23. - 57
See our overview of priority programs.
- 58
"In addition to how we have spent our existing donations you also wanted us to be realistic about having a "response fund" and asked how much ideally would we like in reserves. Well we do in fact need to have such a reserve fund so we an respond to requests for unexpected and urgent projects that come up that we are in the perfect position to assist with if we have the funds available. I guess a sum of up to $50,000 would be the minimum for such a fund.
Some uses we have already planned for and indeed have recently had confirmed funding for such as the hydrocele camps; others we are committed to but still need additional funding to cover in future such as Dr Peg Cumberland's work in Mozambique. Others uses might be extending treatment in some areas, SAFE washing kits for trachoma and LF leg washing (which we respond to as they come in), then there are improved advocacy materials. Finally within the secretariat there are important events such as attending conferences etc for advocacy.
The Givewell donations if they were to come through would hopefully also secure the leverage to use funding for attending meetings in order to advocate on an international stage to further the case for NTDs."
Alan Fenwick, email to GiveWell, November 15, 2011. - 59
"Future commitment as and when funding is available: Angola, $20,000, mapping;
Ethiopia, $30,000, mapping." Schistosomiasis Control Initiative, "Funding of Programmes with Donations from Individuals." - 60
Alan Fenwick, phone conversation with GiveWell, November 15, 2011.
- 61
"When we applied for the DFID grant we promised to deliver 75 million treatments in 5 years from 2011 - 2015. Then in 2011 we agreed to pay for the delivery of treatments in Malawi, Mozambique, Niger, Uganda and Zambia not using drugs purchased by DFID funding but using drugs already in the countries - either from World Vision and/or WHO These amount to approximately 15 million treatments so that means we can deliver &5 +15 = 90 million with the DFID money - but 75 million with drugs purchased by the DFID funding." SCI also notes that as of November 2011, there was a possibility that SCI would receive an additional 18 million treatments over five years from another group. Alan Fenwick, email to GiveWell, November 20, 2011.
- 62
Schistosomiasis Control Initiative, "Grants for 2012 (November 2011)." SCI provided initial estimates of how treatments funded by DFID will be divided among the eight countries in Schistosomiasis Control Initiative, "ICOSA 6-year PZQ Forecast." This document does not include the 18 million treatments donated by World Vision in November 2011.
- 63
- Global Atlas of Helminth Infections, "Malawi."
- Global Atlas of Helminth Infections, "Mozambique."
- Global Atlas of Helminth Infections, "Senegal."
