A note on this page's publication date
The content we created for the Nurse-Family Partnership in 2010 appears below. This content is likely to be no longer fully accurate, both with respect to what it says about the Nurse-Family Partnership and with respect to what it implies about our own views and positions. With that said, we do feel that the takeaways from this examination are sufficient not to prioritize re-opening our investigation of this organization at this time.
Note added June 2024: We are no longer updating reviews of individual organizations outside our Top Charities.
In 2011, we declared the Nurse-Family Partnership a "standout organization," which meant that we found it to be an outstanding opportunity to accomplish good but that we rated our top charities above it.
Published: 2010
Table of Contents
What do they do?
The NFP model consists of having trained registered nurses visit low-income, first-time mothers—starting with weekly visits early in pregnancy, and progressing toward monthly visits until the child's second birthday—attempting to help with prenatal health (nutrition; obtaining prenatal care; and reducing alcohol, tobacco, and drug use during pregnancy), child care, and personal life management (planning future pregnancies and taking steps toward education and employment).1
The Nurse-Family Partnership (NFP) primarily provides a consulting (as opposed to funding or implementing) role, partnering with regional organizations to carry out the NFP program. We present below NFP's activities, along with the associated 2009 expenses (which we cite below as a proportion of the organization's total expenses):2
- Program development (22%): helping regional organizations raise funding and preparing them to deliver NFP services.
- Nursing practice (16%): training and supporting participating nurses.
- Program quality support (16%): ongoing evaluation and consultation with regional programs.
- Federal policy and program finance (7%): advocacy for more government funding of NFP programs.
- Other (40%): administrative and management costs; information technologies; marketing; program research; and a small amount for grants to Colorado NFP agencies.
Does it work?
Evidence of impact
The NFP program has been rigorously evaluated in three studies that found positive, long-term impacts, including less child abuse and neglect,3 and fewer arrests and convictions.4 For more on evidence of effectiveness, see our review of the Nurse-Family Partnership program.
There is reason for caution in extrapolating from the results of these studies to the expected impact of the NFP program as a whole; the question is how well regional programs, working with NFP's help, can replicate the most important aspects of the program. We cannot be fully confident about the quality of replication, but are cautiously optimistic for the following reasons:
- NFP was established with direct involvement from David Olds, the lead researcher on all of the above studies, specifically to replicate the program under discussion.
- NFP has clear, measurable criteria for adherence to the program, including the requirement that registered nurses carry out the program according to the (proprietary) NFP curriculum.5
- As shown in the rigorous studies of the NFP program, empirical evidence for the model's effectiveness holds across very different populations.6
- NFP appears thorough in its ongoing monitoring of its work and the monitoring results we have considered are consistent with positive impact (more on this in the next section).
Ongoing monitoring
The Nurse-Family Partnership monitors outcomes for all clients to determine whether the program is achieving expected results. The Nurse-Family Partnership sent us detailed reports which provide data, including the following indicators (all of which were measured in the earlier, randomized controlled trials):7
- Maternal smoking during pregnancy
- Time between a mother's current pregnancy and her next pregnancy
- Maternal self-sufficiency (as measured by mothers' workforce participation level)
The trends presented in the reports are consistent with the Nurse-Family Partnership having a positive impact:8
- Between intake and the 36th week of pregnancy, self-reported cigarette smoking fell from 14.4% to 12.1% of mothers; drug use from 1.4% to .5%; and, alcohol use from 1.3% to .9%.9
- At intake, 6.1% of mothers reported experiencing physical abuse from her partner; at 36 weeks, only 3.6% reported experiencing physical abuse.10
While we have not analyzed the results in the monitoring reports to determine whether the results the Nurse-Family Partnership is currently achieving are consistent with the trial results, we commend them for their ongoing monitoring of their work and believe that the results we have considered are consistent with a positive impact.
What do you get for your dollar?
According to NFP, the cost to a community/agency is typically $4,500 per family per year served in the NFP program, and ranges from $2,914 to $6,463 per family per year.11 These figures imply a typical cost of $10,800 per family served in the NFP program.12 We don't know how NFP came to the cost figures above and what costs they include to what actors.
According to The Coalition for Evidence-Based Policy, the program costs around $12,500 per woman over the approximately 3 years of visits.13
Room for more funds?
We feel that NFP has room for more funding only over the long term, and that potential donors should take this into account.14
Details: In 2007, NFP launched a campaign to raise money so that NFP could become, over a ten-year period, self-sustaining on the fees it collects from local NFP programs. In 2007, NFP successfully got commitments of approximately $50 million for this purpose, the full amount it sought.15
Since then, NFP has revised its cash flow projections, making the projections less optimistic in light of the weak economy. It has shared these cash flow projections for our eyes only.16 The projections anticipate that donations will be needed for several years to cover the gap between earned revenues (from local NFP programs) and expenses, and that it will take until 2021 to get to the point where earned revenues cover 98% of all expenses.17
From these projections, it appears to us that existing commitments can sustain NFP through 2015, at which point the organization will likely need more donations in order to continue operating.18 It also seems likely to us that any additional donations in the meantime will be essentially “held for a rainy day,” i.e., saved for the point at which they are needed to cover this gap. Because NFP’s goal is to become self-sustaining on earned revenue,19 it seems unlikely that it would use more donations to directly increase the reach of its program (e.g., through providing its services to local NFP offices for free or reduced prices).
We feel that NFP is an outstanding organization, with a stronger case for its effectiveness than any other organization we know of doing work on U.S. equality of opportunity. Therefore, we very much hope that it raises the funds that are necessary to continue operating, and in plenty of time. However, it seems important to note that its need for more funds - and ability to translate them into more outcomes - is fairly far off.
Financials.
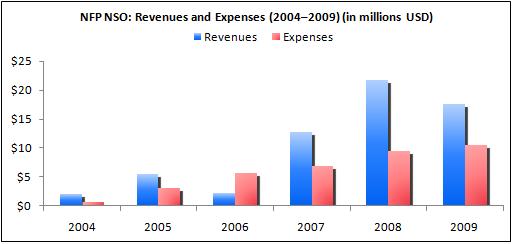
Revenue and expense growth20 (about this metric): NFP's expenses have grown over time, which indicates the program can continue to expand. In the three last years we have data for (2007–2009), NFP got approximately twice as much in revenues as it spent, i.e. in these 3 years, it got around $25 million more than it spent. This relationship between NFP's revenues and expenses makes us worry that NFP is taking in more than it can productively spend.
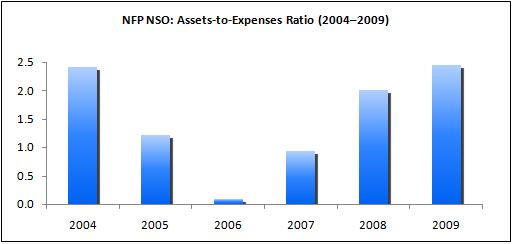
Assets-to-expenses ratio (about this metric): In 2008 NFP NSO had an assets-to-expenses ratio of approximately 2 and in 2009 the ratio was about 2.5.
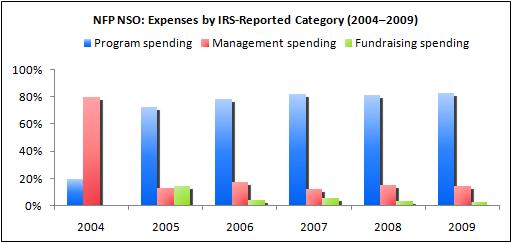
Expenses by IRS-reported category (about this metric): NFP maintains a reasonable "overhead ratio," spending between approximately 73% and 83% of its budget on program expenses in years 2005 to 2009. In 2004, NFP spent much more on "managment and general" than on programs, which we don't think is a problem since this was during a time when NFP was starting up.21
Remaining questions
According to NFP, the cost to a community/agency is typically $4,500 per family per year served in the NFP program, and ranges from $2,914 to $6,463 per family per year.22 We don't know how NFP came to the cost figures above and what costs they include to what actors.
Sources
- Coalition for Evidence-Based Policy, Nurse-Family Partnership. http://evidencebasedprograms.org/wordpress/?page_id=57 (accessed August 23, 2011). Archived by WebCite® at http://www.webcitation.org/619q9JcHI.
- Eckenrode, John, et al. 2010. Long-term effects of prenatal and infancy nurse home visitation on the life course of youths: 19-year follow-up of a randomized trial. Archives of Pediatric and Adolescent Medicine 164: 9-15.
- GiveWell. The Nurse-Family Partnership program.
- National Registry of Evidence-Based Programs and Practices. Nurse-Family Partnership. http://www.nrepp.samhsa.gov/ViewIntervention.aspx?id=88 (accessed November 11, 2010). Archived by WebCite® at http://www.webcitation.org/5uA8OOmAQ.
- Nurse-Family Partnership. Annual report (2007) (PDF).
- Nurse-Family Partnership. Audited financial statements (2008) (PDF).
- Nurse-Family Partnership. Budgets by program department (2005-2008) (PDF).
- Nurse-Family Partnership. Cost-benefit analysis.
- Nurse-Family Partnership. IRS form 990:
- Nurse-Family Partnership. Example implementing agency evaluation report. Our latest information is that this document is classified as confidential by NFP.
- Nurse-Family Partnership. Model elements. http://www.nursefamilypartnership.org/Communities/Model-elements (accessed June 23, 2010). Archived by WebCite® at http://www.webcitation.org/5qhbO6CXY.
- Nurse-Family Partnership. National statistics (2010) (PDF).
- Nurse-Family Partnership. National office program department descriptions and budgets (Actual) (2009) (DOC).
- Nurse-Family Partnership. Program history. http://www.nursefamilypartnership.org/About/Program-history (accessed September 27, 2010). Archived by WebCite® at http://www.webcitation.org/5t386wPZf.
- Nurse-Family Partnership. Summary metrics and financials. NFP has asked us not to publish this document.
- Nurse-Family Partnership. The home visit experience (PDF).
- Nurse-Family Partnership. Theory of change logic model (PDF).
- Nurse-Family Partnership. What we do. http://www.nursefamilypartnership.org/about/what-we-do (accessed June 23, 2010). Archived by WebCite® at http://www.webcitation.org/5qhZz0hIS.
- Olds, David L., et al. 1997. Long-term effects of home visitation on maternal life course and child abuse and neglect: Fifteen-year follow-up of a randomized trial. Journal of the American Medical Association 278: 637-643.
- Stapleton, Michelle. NFP Fund Development Associate. Email to GiveWell, November 16, 2010.
- Stapleton, Michelle. NFP Fund Development Associate. Phone conversation with GiveWell, July 21, 2010.
- 1
Nurse-Family Partnership, "What We Do."
Nurse-Family Partnership, "Model Elements."
"Home visits weekly the first month following program
enrollment, then every other week until birth of infant.... Home visits weekly during postpartum period, every 2 weeks until toddler is 21 months, monthly until child is 2 years." Nurse-Family Partnership, "Theory of Change Logic Model," Pg 1. - 2
Nurse-Family Partnership, "National Office Program Department Descriptions and Budgets (Actual; FY 2009)."
- 3
The publication from follow up when the children are 15 years old is Olds et al. (1997). When considering the full sample, it finds only one statistically significant (at 5% significance level) effects on mothers and child abuse and neglect of NFP: the families who got nurse-visits had fewer substantiated reports of child abuse and neglect. The average incidence was 0.29 in the treatment group and 0.54 in the control group (P0.01).
- 4
The publication for the follow up when the children are 19 years old is Eckenrode et al. (2010). When considering the whole sample, it finds the following statistically significant (at 5% significance level) effects of NFP on the 19-year olds:
- Fewer youth ever arrested (risk ratio 0.57 [95% CI: 0.35-0.93]; 21% in treatment vs 37% in control)
- Fewer youth ever convicted (risk ratio 0.42 [95% CI: 0.20-0.90]; 12% in treatment vs 28% in control)
- Fewer arrests in lifetime (incidence risk ratio 0.43 [95% CI: 0.23-0.80]; mean in treatment group 0.37, mean in control group 0.86)
- Fewer convictions in lifetime (incidence risk ratio 0.34 [CI:0.15-0.79]; mean in treatment group 0.20, mean in control group 0.58)
- 5
Unfortunately, Nurse-Family Partnership, "Example implementing agency evaluation report," which gives a good sense of these criteria, is confidential.
- 6
Quotes from Coalition for Evidenc-Based Policy, "Nurse-Family Partnership," describing the samples in the three RCTs of the NFP program:
- "Study 1 (Elmira, New York)
This was a randomized controlled trial of 300 women in Elmira, New York, a semi-rural community.... Approximately 90% of the women were white, 60% were low income, and 60% were unmarried. Their average age was 19." - "Study 2 (Memphis, Tennessee)
This was a randomized controlled trial of 743 women in Memphis, Tennessee.... Approximately 90% of the women were African-American, 85% came from households with income at or below the poverty line, and almost all were unmarried. Their average age was 18." - "Study 3 (Denver, Colorado)
This was a randomized controlled trial of 490 women in Denver, Colorado.... These women were almost all low-income (their annual household income averaged $17,800 in 2008 dollars), 46% were Mexican American, 36% were white, 15% were African American, and 84% were unmarried. Their average age was 20."
- "Study 1 (Elmira, New York)
- 7
Information on what the randomized controlled trials evaluated from National Registry of Evidence-Based Programs and Practices, "Nurse-Family Partnership."
Nurse-Family Partnership indicators in Nurse-Family Partnership, "National Statistics (2010)."
- 8
The following data cover the full period of program implementation from 1996 to July 31, 2010 (when Nurse-Family Partnership sent GiveWell this file.) " This report presents analysis of data available from program initiation in 1996 through July 31, 2010, and covers the pregnancy, infancy and toddler phases of the program." Nurse-Family Partnership, "National Statistics (2010)."
- 9
Nurse-Family Partnership, "National Statistics (2010)."
Note we have not seen a technical report that defines these terms.
- 10
Nurse-Family Partnership, "National Statistics (2010)."
- 11
"Following is information about the average cost of a family in the NFP program to a community/agency and is approved for public dissemination:
Nurse-Family Partnership typically costs $4,500 per family per year with a range throughout the country of $2,914 - $6,463 per family per year based primarily on variations in costs of living." Michelle Stapleton, e-mail to GiveWell, November 16, 2010.
- 12
$4,500 * 2.4 = $10,800
- 13
"The program costs approximately $12,500 per woman over the three years of visits (in 2010 dollars)." Coalition for Evidence-Based Policy, "Nurse-Family Partnership."
- 14
We published a blog post on the room for more funding of NFP, similar in content to this section. You can access the blog post here.
- 15
"In April 2007 Nurse-Family Partnership National Service Office launched a campaign to raise $50 million to advance our 10-year growth strategy and to make operations self-sustainable. We are honored to announce that in the past year we have received commitments from private foundations and individual donors meeting our campaign goal of $50 million. The funding will support organizational infrastructure. Programmatic support will still be needed from government agencies at federal, state, and local levels to make services available to specific communities and states. The commitments, made primarily in the form of grants, are multi-year and are tied to annual performance goals integral to the 10-year strategic growth plan. Additional funding has been committed by Nurse-Family Partnership’s board of directors." Nurse-Family Partnership, "Annual Report (2007)," Pg 31.
"As far as funding goes, there are two kinds I should address. One is that the national office launched a growth capital campaign in 2007 with the goal of raising $50 million to fund growth over the next ten years to the point where we’re economically self-sufficient at NFP National Service Office, with the exception of special projects we might have. Of that $50 million, 100% has been committed by a group of co-investors: The Edna McConnell Clark Foundation, Bill & Melinda Gates Foundation, Robert Wood Johnson Foundation, W. K. Kellogg foundation, The Kresge Foundation, Robertson Foundation, and NFP Board of Directors. The NFP Board of Directors committed $8 million of the $50 million and we’re a little over halfway to raising the board commitment....
GiveWell: Are you still fundraising or have you raised what you need?NFP: The $50 million has been committed but we still have $3.5 million [of the board commitment] that has to be raised. The board committed to give or get the $8 million and we’re helping them to reach that goal.
With that said, the recession wasn’t something we planned for in 2007. So, we’ve revisited our business plan and growth goals in a world where we have 2-3 years of slower than we anticipated growth, and that takes our initial 10-year timeline out a few more years and requires more funding. The initial growth model was to cover us for 10 years. Now, that we’re expecting it to take 12-13 years to become self-sustaining, we’ll need an additional $8-10 million for those extra 2-3 years (in addition to the $3.5 million that is committed by the board but not raised).
GiveWell: Can you explain more about the fees you receive from local NFP programs?
NFP: Local NFP programs pay the NFP National Service Office to educate the nurses—each nurse goes through a set curriculum. Local NFP programs also pay us technical assistance fees on an ongoing basis. You can see it in the budget you have, even though it’s slightly outdated, that those fees cover ongoing education, direct nurse consultation, reporting and data services that we provide to the agencies.
GiveWell: So the goal is to raise money to sustain you to the point where you’re funded just by fees from local programs?
NFP: Correct." Michelle Stapleton, phone conversation with GiveWell, July 21, 2010.
- 16
Nurse-Family Partnership, "Summary Metrics and Financials."
- 17
Nurse-Family Partnership, "Summary Metrics and Financials."
- 18
Nurse-Family Partnership, "Summary Metrics and Financials."
- 19
"GiveWell: So the goal is to raise money to sustain you to the point where you’re funded just by fees from local programs?
NFP: Correct." Michelle Stapleton, phone conversation with GiveWell, July 21, 2010.
- 20
The data on NFP's revenues and expenses comes from
Nurse-Family Partnership, "IRS Form 990 (2004)."
Nurse-Family Partnership, "IRS Form 990 (2005)."
Nurse-Family Partnership, "IRS Form 990 (2006)."
Nurse-Family Partnership, "IRS Form 990 (2007)."
Nurse-Family Partnership, "IRS Form 990 (2008)."
Nurse-Family Partnership, "IRS Form 990 (2009)." - 21
"The Nurse-Family Partnership National Service Office, a national non-profit, was established in 2003." Nurse-Family Partnership, "Program History."
- 22
"Following is information about the average cost of a family in the NFP program to a community/agency and is approved for public dissemination:
Nurse-Family Partnership typically costs $4,500 per family per year with a range throughout the country of $2,914 - $6,463 per family per year based primarily on variations in costs of living." Michelle Stapleton, e-mail to GiveWell, November 16, 2010.
