In March 2014, Nyaya Health changed its name to Possible (http://possiblehealth.org/). This page, which was completed in 2011, uses the name Nyaya Health.
A note on this page's publication date
The content we created for Nyaya Health in 2011 appears below. This content is likely to be no longer fully accurate, both with respect to what it says about Nyaya Health and with respect to what it implies about our own views and positions. With that said, we do feel that the takeaways from this examination are sufficient not to prioritize re-opening our investigation of this organization at this time.
Note added June 2024: We are no longer updating reviews of individual organizations outside our Top Charities.
In 2011, we declared Nyaya Health a "standout organization," which meant that we found it to be an outstanding opportunity to accomplish good but that we rated our top charities above it.
Published: July 2011
Summary
Nyaya Health operates a hospital and system of community health workers in partnership with the government in the district of Achham, Nepal.
We feel that Nyaya Health is a standout organization because of its:
- focus on providing basic health care in a very poor location, an approach we find promising.
- unusual transparency - Nyaya Health shares an unusual amount of information about its operations publicly.1
Our full review, below, discusses our full assessment of Nyaya Health, including what we see as its strengths and weaknesses as well issues we have yet to resolve.
Update
In May 2012, Nyaya Health provided the following updated information, which we have not yet reviewed:
- Overview letter (PDF)
- Progress to date (April 2012) (PDF)
- Organizational updates (PDF)
- Tools of transparency and processes (PDF)
- Funding scenarios (FY2012-2013) (PDF)
- Nepal and U.S.-based operations budgets:
- May 2012 versions: Nepal operations budget and U.S.-based operations budget
- Versions that may incorporate more recent changes: https://www.dropbox.com/sh/sr384lfpy4pg3uu/PmpoSn5nwP
Our review process
Our evaluation of Nyaya Health consisted of reviewing publicly available information, speaking by phone with Nyaya Health board members and volunteers, and reviewing information that Nyaya sent to us in response to our questions.
Table of Contents
- A note on this page's publication date
- Summary
- What do they do?
- Does it work?
- What do you get for your dollar?
- Room for more funds?
- Unresolved issues
- Sources
What do they do?
Nyaya Health operates a hospital and system of community health workers in the district of Achham, Nepal.2
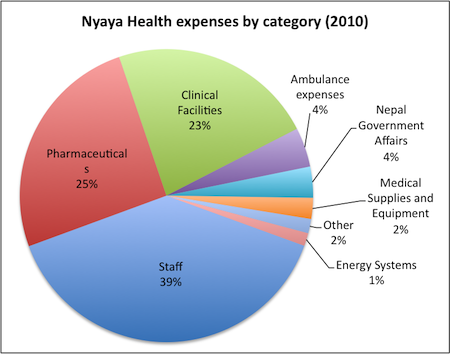
Nyaya Health is a small organization. It spent $162,494 in 2010.3
It provides a break down of its expenses:4
Services
Below, we provide basic figures for Bayalpata Hospital for the period of January 15, 2010 to December 15, 2010. Nyaya Health does not have hospital registries for before this period:5
- Admitted 772 patients
- Provided care for 1541 inpatient days
- Served 18,914 outpatients
- Served 1,897 emergency patients
- Provided 106 X-Rays (starting in November 2010)6 and 612 ultrasounds
- Had 108 deliveries
- Did 14,168 lab tests
- Served 114 neonatal patients
- Enrolled 79 HIV patients on therapy (starting in July 2010)7
- Performed 288 abortions
Nyaya has also shared data from a limited time period (February 15 – April 15, 2011) on the primary diagnoses of patients seen at the hospital (see footnote).8
Nyaya Health also provides ambulance services.9
Staff
According to Nyaya Health's website, its hospital is staffed by 24 Nepalese employees, including a doctor, 6 midwives, 4 health assistants and aides, 4 Community Health Workers, a lab assistant, an x-ray aide, an ambulance driver, and 6 support staff.10 Nyaya Health informed us that as of March 2011, it employed an additional doctor, as well as 45 Female Community Health Volunteers (FCHVs) under the leadership of the Community Health Workers.11 Nyaya gives details of where each staff member received his/her training and what he/she did before working for Nyaya.12
Does it work?
In our view, the key questions for Nyaya Health's effectiveness are:
- Does Nyaya Health's presence increase utilization of health services (by improving accessibility for the local population)? Nyaya conducted an informal survey of conditions before it entered Achaam, but neither we nor Nyaya believe that this survey is representative of what current conditions would be like in Nyaya's absence. In addition, Nyaya sent us a document (discussed below) focused on answering this question, specifically. Given that there is a government district hospital in the same region as Nyaya's facility, and we don't know the degree to which Nyaya's and the district hospital's populations served overlap, we do not feel we have sufficient information to answer this question.
- What is the quality of care that Nyaya Health provides? We'd guess that the quality is at least acceptable, based on our impression that Nyaya has regular visits from developed-world health professionals (and based on statements from these visitors). We also draw some encouragement from Nyaya's unusual degree of public reporting.
Does Nyaya Health's presence increase utilization of health services (by improving accessibility for the local population)?
We have limited information to answer this question. Nyaya Health conducted an informal assessment of the health and available services in the area before starting its work, consisting of "site visits to several of the health posts, hospitals, private medical offices, pharmacies, and government offices in the region [and interviews with] 1) administrators, politicians, leaders, local headmasters; 2) community-based outreach workers; 3) healthcare providers, health assistants, midwives, pharmacists, private practitioners; 4) members of the target population."13
However, at the time the survey was conducted, Achham was likely in a particular poor position due to the end of a 10-year-long civil war in 2006.14
The Nepali government has improved the district hospital15 that was minimally staffed and inaccessible when Nyaya Health entered Achham, and we have little information regarding the degree to which the populations served by Nyaya Health and the district hospital overlap.
Nyaya Health also sent us a document stating that the Nepal Ministry of Health allocates doctors on a per-facility rather than on a per-area or per-person basis. The document shows that Achham has 4 full-time doctors while two other nearby districts have 2 and 1 respectively.16 This document does not resolve our question about the counterfactual because it is unclear to us (a) whether additional doctors led to patients receiving services that they would not have otherwise received; and (b) whether the Ministry of Health would have staffed this second hospital (i.e., the one Nyaya now operates) on its own if Nyaya did not exist.
What is the quality of care that Nyaya Health provides?
We see two reasons to be cautiously optimistic about the quality of Nyaya Health's care: (a) it has told us that it has frequent visits from developed-world medical professionals unaffiliated with Nyaya Health; (b) Nyaya Health publicly reports an unusual degree of information on its outcomes, including poor outcomes.
Visits from developed-world medical professionals
Nyaya Health stated to us that its site is fairly regularly visited by developed-world medical professionals.17 Were we to continue our review, we would seek additional information on how often Nyaya has had outside visitors in the past and what their experiences have been.
The following are accounts of visits to Nyaya Health's facilities in Achham by medical professionals who are not employed by or on the board of Nyaya Health. Because these accounts are by self-selected people (people who chose to invest time and money to travel to Nyaya) and because in many cases their accounts were chosen for public posting by Nyaya Health, they are not unbiased accounts. Names and brief biographies are below; quotes follow in footnotes.
- In November 2010, Dr. Michael Polifka, an American physician with six years of international medical volunteering experience, spent two weeks working with the staff of Bayalpata Hosptial. Dr. Polifka told us by phone that of the 15-20 international health organizations he has worked with Nyaya is "unequivocally at the top" in terms of continuous striving for the very best quality of care and that they are also rigorous about using all donated funds efficiently and without waste. Dr. Polifka told us that cases he saw handled well included numerous cases of pneumonia and diarrhea among children, trauma cases, chronic medical problems and cases of tuberculosis, leprosy, and acute tetanus. Dr. Polifka plans to return to the Bayalpata Hospital every six months for 3-4 weeks at a time.18
- Dr. Ruma Rajbhandari is a Nyaya Health volunteer. She has a MD and MPH from Harvard Univerity and is a resident physician in Internal Medicine at Brigham and Women’s Hospital in the Global Health Equity Residency program. She has visited/worked in a number of rural, developing-world hospitals, has been to the Nyaya Health hospital twice, and plans to make annual trips. She told us, "Nyaya Health provides a much higher quality of care than most government-run district hospitals particularly those government facilities located in the Far-Western region of Nepal where Nyaya is located…. For the conditions that Nyaya Health is able to provide services for, it does a good job."19
- A Norwegian "occupational physician" named Knut Skyberg visited Nyaya's hospital and blogged about his experiences in November 2010, but did not describe observing care being delivered.20
- Dr. Prativa Pandey, the director of a clinic in Kathmandu, visited the hospital, wrote about her experiences, and made a donation to Nyaya Health. She noted a number of issues with the facility including poor quality of the buildings and lack of equipment, but also noted, "Bayalpata Hospital seemed to be well staffed by motivated people."21
- A physician from Vermont visited the hospital and reported on the medical conditions he observed, but not the care he saw patients receive. He wrote, "The hospital can do plain x-rays and very simple chemistries and diagnose TB sputum samples. Anything more complicated requires referral to bigger facilities that are 6 to 20 hours away by jeep."22
Public reporting on medical outcomes
Nyaya posts detailed reports on some of the morbidity and mortality cases that occur at its facilities. Nyaya told us that, since July 2010, its staff have examined one case each week and sent their reports to an email list of 15 medical professionals working in Nepal, the U.S., and elsewhere for review and comments.23 As of April 1, 2011, there were 20 reports online dated after July 22, 2010 (as well as six mortality reports from before this period), over a span of 36 weeks. We summarize the first 16 cases since the start of the morbidity and mortality review program and some of the problems Nyaya Health identifies in each report (see footnote; note that we have not yet reviewed the more recent reports).24
Possible negative/offsetting impact
As stated at our discussion of impact analysis, we are generally concerned about charities' potential diversion of skilled labor, interference with government responsibilities, and/or diversion of limited government funding.
These concerns are difficult to systematically evaluate and/or quantify. Below are Nyaya Health's statements on these concerns.
Possible diversion of skilled labor: Nyaya Health told us:
- In urban areas in Nepal there is no shortage of doctors and surgeons.25 As discussed above, there was very little medical care available in Achham prior to Nyaya Health's involvement. Therefore, shifting a doctor from an urban area to Achham could add capacity where it did not exist before while not reducing it elsewhere.
- If staff were not working at Bayalpata Hospital, they would likely be working as private health care providers in local towns, at a local health post, or would have migrated to other regions. Nyaya Health notes, "Private 'medicals' and health posts in the region are unregulated and typically provide poor-quality care and medicines, and have high rates of absenteeism and stock-outs. It is our hope that by bolstering the public sector health facilities in the region we can decrease the number of health workers providing unregulated care in such facilities and we have seen at least anecdotal evidence of such."26
We remain concerned about the possibility that medical staff may be drawn from limited pool of staff willing to work in rural areas.
Possible interference with government services: Nyaya Health reports (above) that government health services were largely non-existent in the area prior to Nyaya Health's arrival. Nyaya Health also notes that government investment in health in the region has increased since its arrival, and has not increased at the same rate in surrounding regions (we have not seen data on this).27
Possible diversion of limited government funding: Nyaya Health receives funding from the government of Nepal.28
We worry that these funds may have been reallocated from other regions in Nepal, rather than being additional investments in health. It is possible that while funding may have been reallocated from other regions, this may have resulted in more funding going to regions with greater needs.29
We have not been able to determine whether this is the case, as we have not seen data on health spending by region over time. Nyaya notes:30
Other concerns: We also asked Nyaya Health about potential sources of reduced impact, specifically security concerns and its geographic isolation. Nyaya Health told us that security has not been a concern to date and that the location for the hospital was chosen because it is "centrally located for a very rural and dispersed population." However, "Achham is an extremely rural area with limited roads/transport access and the population is very poor making travel even more challenging."31
What do you get for your dollar?
We have not completed a cost-effectiveness estimate for Nyaya Health.
Because it provides comprehensive care, Nyaya is likely not as cost-effective in a $-per-lives-saved or per-DALYs-averted sense as programs that distribute vaccines or bednets. We weigh cost-effectiveness among other considerations when evaluating a charity, though we try not to put undue weight on this one factor. (For more, see our perspective on using cost-effectiveness metrics).
Room for more funds?
Update: In May 2012, Nyaya Health provided updated budgets for its Nepal and U.S.-based operations and updated funding scenarios (see above). We have not yet reviewed these documents.
Nyaya Health's funding gap for 2011 is estimated at $85,000 and for 2011-2013 at about $920,520. Details below.
Short-term projections: 2011
Nyaya Health told us on March 14, 2010:32
As of June 2011, it appears that Nyaya has raised about $315,000 of the target $400,000 for 2011.33 Thus, we estimate Nyaya's funding gap for 2011 at $85,000.
Nyaya Health provides regular updates on its website on how much it has in the bank.34
Nyaya Health provided details of what it would do at each level of funding:35
- Additional $100,000-200,000 fundraised by end of FY2011 (This had been raised as of June 2011.)
- Clinical: Continue to run currently available services, expand inpatient beds from 12 to 25, add isolation ward for infectious patients, add overnight nurses station, expand obstetrical services from one to three rooms, expand emergency from four to six beds, add on-call room for overnight ER staff, and renovate outpatient department to include five individual rooms.
- Community outreach: Continue community health services in four villages and expand to an additional six villages.
- Facilities: Annual maintenance and renovation of two additional staff quarters.
- Power: Complete installation of solar energy to cover 30% of total electrical needs.
- Additional $200,000-300,000 fundraised by end of FY2011 (This had been raised as of June 2011.)
- Clinical: All of the above plus comprehensive surgical services, emergency blood banking services, and expanded laboratory capacity including microbiological culture facilities.
- Community outreach: All of the above plus initiation of community preventive health educational programs in schools and community institutions.
- Facilities: All of the above plus renovation of an additional staff building.
- Power: Same as above.
- Additional $300,000-400,000 fundraised by end of FY2011 (As of June 2011, we estimate that Nyaya had raised an additional $315,000.)
- Clinical: All of the above plus nutritional support programs for malnourished and chronic disease patients, Intensive Continuing Medical Education programs for all clinical staff members, and initiation of dentistry services.
- Community outreach: All of the above plus expand to an additional six villages.
- Facilities: All of the above plus construction of a new perimeter fence around hospital grounds, erosion-prevention retention walls, blacktop road from main road to buildings on hospital grounds, roofing over walking/stretcher paths, and expanded piped water systems to all hospital building with on-site reservoir.
- Power: Same as above with possibility of adding additional solar panels.
- Additional $400,000+ fundraised by end of FY2011
- "Were we to raise this amount of money by the end of FY2011, further discussions will be needed at that time in order to evaluate our priorities subsequent to this afore-mentioned list. While clearly an amazing opportunity for our work for the people of Achham, we will likely need to recruit new on-site managerial, clinical, and community staff members in order to expand and maintain services at a rate commensurate with this amount of funding."
Extended expansion: 2011-2013
Nyaya Health provided a budget for its expansion plans over 2011-2013. Expansion costs and expected outputs included:36
- Surgical and blood banking expansion: is projected to cost a total of $307,786 over 2011-2013, including both capital and operating costs. This amount would account for 29% of Nyaya's planned expansion. Under this plan, Nyaya estimates that it would be able to provide 4,378 minutes of operating room time per year and serve 40% of demand for surgical services in 2013 (with more limited capacity in 2011-2012). Nyaya estimates that one surgery takes between 30 and 130 minutes, depending on the type and age of patients.37
- Community health expansion: Nyaya plans to spend an estimated additional $288,321 on its community health program (providing community health workers to the surrounding area) over 2011-2013.38 This amount would account for 27% of Nyaya's planned expansion.39 Under this plan, it would serve 60 village development committees in 2013 (up from 9 in 2011), and have 720 female community health volunteers (up from 108 in 2011). 40
- General expenses: Nyaya expects to need an additional $208,035 over 2011-2013 for general hospital expenses, 17% of the planned expansion.41 These costs are labeled "office supplies" in its planning document.42
- Outpatient and inpatient expenses: Nyaya projects that its outpatient expenses will grow by $104,198 and its inpatient expenses will grow by $99,851 over the course of 2011-2013, 10% and 9% respectively of the planned expansion.43 It expects to provide 36,000 outpatient visits per year in 2013 (up from 13,500 in 2011) at a cost of a little over a dollar per visit, and to cover 40% of the demand for this service.44 It expects to serve 3,000 inpatients per year in 2013 (up from 600 in 2011) at a cost of about $6.30 per day, and to cover 50% of the demand for this service.
- Other additional costs: Nyaya Health expects to spend an additional $95,728 on laboratory, radiology, obstetric, and emergency services over the course of 2011-2013, 9% of the total expansion.
Nyaya Health's total expansion in 2011-2013, were it to receive sufficient funding, would cost $1,073,026. Above, we estimate that Nyaya has raised about $315,000 in the first half of 2011, or about $152,500 more than the amount needed to cover expenses at the 2010 level of operations. Thus we estimate that Nyaya has a funding gap for its 2011-2013 expansion of $920,520.45
Unresolved issues
In evaluating Nyaya Health, we sought to understand the counterfactual: what health services would exist in the area Nyaya operates if it did not exist? We have not been able to answer this question with high confidence.
In addition, we have not fully answered the following questions:
- Impact. How has health in Achham changed as a result of Nyaya Health's involvement in the area? Have lives been saved/improved as a result of Nyaya Health's activities? How many lives?
- Other access to free care. Nyaya Health told us that it is the only facility in the area providing free care46 ; however independent sources discuss a national program to provide free care at public hospitals and health centers.47 What is the current and projected reach of the national program?
- Cost effectiveness. How much has Nyaya spent per life saved/improved in the past? What is the value of the additional activities/investments in terms of lives saved/improved?
- Negative/offsetting impact. What would Nyaya Health staff be doing if they weren't working for Nyaya Health? Where would government funding be going if it weren't going to Nyaya?
Sources
- Chin, Brian, Livia Montana, and Xavier Basagña. 2011. Spatial modeling of geographic inequalities in infant and child mortality across Nepal. Health & Place doi:10.1016/j.healthplace.2011.04.006. Abstract available at http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6VH5-52RXVFB-….
- GiveWell. Nyaya Health cost effectiveness calculation (XLS).
- GiveWell. Nyaya Health expenses (2010) (XLS).
- GiveWell. Nyaya Health funding gap analysis (XLS).
- GiveWell. Nyaya Health outputs over time.
- GTZ. Free health care in Nepal: Findings of a rapid assessment (PDF).
- Lichtenstein, Mark, and Cynthia West. 2011. Majestic mountains, fabulous food, a diverse population and amazing illnesses (PDF). The Hardwick Gazette, February 9.
- Maru, Duncan. Nyaya Health Co-Founder and President. Phone conversation with GiveWell, March 17, 2011.
- Nyaya Health. Access database export samples.
- Nyaya Health. Annual report (2010) (PDF).
- Nyaya Health. ART enrollment by month.
- Nyaya Health. Bayalpata Hospital at the crossroads: Update from Achham. http://blog.nyayahealth.org/2011/01/31/weeklyreflection1/ (accessed March 28, 2011). Archived by WebCite® at http://www.webcitation.org/5xWVJktCM.
- Nyaya Health. Budget. http://wiki.nyayahealth.org/w/page/4682609/Budget (accessed January 26, 2011). Archived by WebCite® at http://www.webcitation.org/5w1wfSHK7.
- Nyaya Health. Calculations for Chaitra 2067. We have not yet requested permission to publish this.
- Nyaya Health. Calculations for Falgun 2067. We have not yet requested permission to publish this.
- Nyaya Health. Cases. https://www.dropbox.com/s/dpa8o5e8r0pkvwv#view:list (accessed April 4, 2011). Archived by WebCite® at http://www.webcitation.org/5xh462sk8.
- Nyaya Health. Comments on GiveWell draft review of Nyaya Health.
- Nyaya Health. Delivery data (July 2009 to April 2011) (XLS).
- Nyaya Health. Developing an X-ray program in Achham. http://blog.nyayahealth.org/2010/11/10/xrayprogram/ (accessed March 14, 2011). Archived by WebCite® at http://www.webcitation.org/5xB8nJLXK.
- Nyaya Health. Differential funding scenarios (2011) (DOC).
- Nyaya Health. Expansion costing (XLS).
- Nyaya Health. Financial statements (2009) (PDF).
- Nyaya Health. GiveWell HMIS summary.
- Nyaya Health. Health services assessment in five village development committee areas surrounding Sanfe Bagar, Achham (PDF).
- Nyaya Health. Homepage. http://www.nyayahealth.org/ (accessed January 25, 2011). Archived by WebCite® at http://www.webcitation.org/5w0b45mHZ.
- Nyaya Health. Inpatient and emergency visits and deaths (July 2009-January 2011).
- Nyaya Health. Interview with Dhan Bahadur Bogati. http://blog.nyayahealth.org/2010/08/18/dhanbogarti/ (accessed January 26, 2011). Archived by WebCite® at http://www.webcitation.org/5w1t7mcF0.
- Nyaya Health. Interview with Nyaya Health donor Dr. Prativa Pandey of CIWEC Clinic. http://blog.nyayahealth.org/2009/12/22/prativa_pandey_interview/ (accessed March 3, 2011). Archived by WebCite® at http://www.webcitation.org/5wvBhXpsn.
- Nyaya Health. M&M: 30 y/o Infected Abortion (January 17, 2011) (DOC).
- Nyaya Health. M&M: 60 y/o male with TB (January 24, 2011) (DOC).
- Nyaya Health. M&M review (August 25, 2010) (DOC).
- Nyaya Health. Manual placenta removal (September 30, 2010) (DOC).
- Nyaya Health. Maternal outcomes. http://wiki.nyayahealth.org/w/page/4682710/Maternal_Outcomes (accessed January 27, 2011). Archived by WebCite® at http://www.webcitation.org/5w3GIDCQw.
- Nyaya Health. MMC: 12 and 6 year old brothers dead of unknown poisoning (July 27, 2010) (PDF).
- Nyaya Health. Molar pregnancy vs. incomplete abortion (November 5, 2011) (DOC).
- Nyaya Health. Morbidity review: Suicide attempt by 28 year-old male (August 10, 2010) (DOC).
- Nyaya Health. Mortality and morbidity reviews. https://docs.google.com/leaf?id=0B9ZQBHyI2oBYODQxMDI3NzQtZjAwMC00YmI3LT… (accessed January 26, 2011). Archived by WebCite® at http://www.webcitation.org/5w2Icc9xH.
- Nyaya Health. Mortality reivew: 11 month old with severe acute malnutrition and diarrhea (January 31, 2011) (DOC).
- Nyaya Health. Mortality Review: 17yo male with head trauma (February 7, 2011) (DOC).
- Nyaya Health. Mortality review: Collapse and demise in a village 24 hours from the hospital (September 9, 2009) (PDF).
- Nyaya Heatlh. Mortality review: COPD (PDF).
- Nyaya Health. Mortality review: Death of a four-month old (October 19, 2009) (PDF).
- Nyaya Health. Mortality review: Death of a four-year-old (November 9, 2009) (PDF).
- Nyaya Health. Mortality review: Infant death (June 20, 2010) (PDF).
- Nyaya Health. Mortality review: Intrauterine fetal demise (April 16, 2010) (PDF).
- Nyaya Health. Mortality report: Intrauterine fetal demise in a 20yo primagravid (July 22, 2010) (DOC).
- Nyaya Health. Mortality review: Kala-azar (DOC).
- Nyaya Health. Mortality review: Motor vehicle death (September 17, 2010) (DOC).
- Nyaya Health. Mortality review: Septic shock (September 6, 2010) (DOC).
- Nyaya Health. Non-OPD data: Mortality. http://spreadsheets.google.com/pub?key=p-TJjzE7A-O4wT-vh-N_0Rw&single=t… (accessed January 26, 2011). Archived by WebCite® at http://www.webcitation.org/5w2G8rcl6.
- Nyaya Health. Nyaya Health budget. http://spreadsheets.google.com/pub?key=0AtZQBHyI2oBYcC1USmp6RTdBLU83dnZ… (accessed January 26, 2011). Archived by WebCite® at http://www.webcitation.org/5w1zhwDKV.
- Nyaya Health. Nyaya Health opens Bayalpata Hospital in Achham. http://blog.nyayahealth.org/2009/06/21/bayalpata_opening/ (accessed March 28, 2011). Archived by WebCite® at http://www.webcitation.org/5xWuJfntv.
- Nyaya Health. Nyaya Health’s impact: A framework for evaluation (DOC).
- Nyaya Health. Nyaya Health’s impact in public-sector strengthening: Addressing the counter-factual hypothesis.
- Nyaya Health. Nyaya raises $75,000 to be matched by Nick Simons Foundation in 2 months! http://blog.nyayahealth.org/2011/06/08/nsimatchinggrantfinal/ (accessed June 8, 2011). Archived by WebCite® at http://www.webcitation.org/5zIMNV7Yt.
- Nyaya Health. Outpatient data. http://spreadsheets.google.com/pub?key=0AtZQBHyI2oBYcC1USmp6RTdBLU83N29… (accessed January 26, 2011). Archived by WebCite® at http://www.webcitation.org/5w2D7Iywo.
- Nyaya Health. On rights and retention. http://blog.nyayahealth.org/2010/08/20/rightsandretention/ (accessed January 26, 2011). Archived by WebCite® at http://www.webcitation.org/5w1qny8vz.
- Nyaya Health. Orthopedics in Achham. http://blog.nyayahealth.org/2011/01/24/orthopedics-in-achham/ (accessed January 25, 2011). Archived by WebCite® at http://www.webcitation.org/5w0f0Iqc6.
- Nyaya Health. Overview. http://www.nyayahealth.org/overview/ (accessed January 25, 2011). Archived by WebCite® at http://www.webcitation.org/5w0dkJskp.
- Nyaya Health. Personnel. http://www.nyayahealth.org/personnel/ (accessed February 7, 2011). Archived by WebCite® at http://www.webcitation.org/5wKKCszC6.
- Nyaya Health. Report of ambulance services at Bayalpata Hospital. Nyaya Health asked that we keep this document confidential as it relates to a government project.
- Nyaya Health. Support Nyaya this Holiday season. http://blog.nyayahealth.org/2010/12/17/nyayaholidayseason2010/ (accessed January 27, 2011). Archived by WebCite® at http://www.webcitation.org/5w3Poa6y6.
- Nyaya Health. “We can only take the severely injured right now…” http://blog.nyayahealth.org/2011/03/12/roadaccident/ (accessed March 14, 2011). Archived by WebCite® at http://www.webcitation.org/5xB4hbG5F.
- Nyaya Health. Weighing petrol vs. life: Bayalpata’s continuing energy crisis. http://blog.nyayahealth.org/2010/07/31/solarenergy/ (accessed January 26, 2010). Archived by WebCite® at http://www.webcitation.org/5w1vFPZJV.
- Polifka, Michael. Nyaya Health volunteer physician mentor. Phone conversation with GiveWell, March 14, 2011.
- Rajbhandari, Ruma. Nyaya Health volunteer and Resident Physician at Brigham and Women’s Hospital. Phone conversation with GiveWell, March 18, 2011.
- Republica. 54 health centers without doctors. http://myrepublica.com/portal/index.php?action=news_details&news_id=288… (accessed March 28, 2011). Archived by WebCite® at http://www.webcitation.org/5xWgeHI3m.
- Schwarz, Dan. Nyaya Health Executive Director. Email to Ryan Schwarz, April 7, 2011.
- Schwarz, Ryan. Nyaya Health Director of Operations. Email to GiveWell, March 14, 2011.
- Schwarz, Ryan. Nyaya Health Director of Operations. Phone conversation with GiveWell, February 17, 2011.
- Schwarz, Ryan. Nyaya Health Director of Operations. Phone conversation with GiveWell, March 31, 2011.
- Sinclair, Cameron. Visiting Nyaya Health in Sanfebagar, Nepal (accessed March 4, 2011). The Department of Small Works, January 15, 2008. Archived by WebCite® at http://www.webcitation.org/5wvtIas2r.
- Wikipedia. Nepalese Civil War. http://en.wikipedia.org/wiki/Nepalese_civil_war (accessed June 17, 2011). Archived by WebCite® at http://www.webcitation.org/5zVeGuKeY.
- 1
- Nyaya posts detailed reports on some of the morbidity and mortality cases that occur at its facilities. See Nyaya Health, "Cases."
- Nyaya posts highly detailed spending information. See Nyaya Health, "Nyaya Health Budget."
- Starting in March 2011 (and for a limited earlier period), Nyaya has posted data on inpatient, outpatient, and emergency patient diagnoses. See Nyaya Health, "Outpatient Data," Sheets OPD Disease Codes, IPD Disease Codes, and ED Disease Codes.
- 2
Nyaya Health’s activities in Achham are centered at the Bayalpata Hospital. The hospital, run as a collaboration between Nyaya Health, local citizens, and the Nepali government, centers around a model of comprehensive primary care, including maternal and child health, infectious disease prevention and treatment, and management of chronic conditions for an expanding catchment population of a quarter million people. The hospital is located in the major transit hub for the region and treats over 3,000 patients per month on average. It is run by over twenty Nepali staff including physicians, community healthcare workers, nurse midwives, lab technicians, pharmacists, and project managers. The hospital includes a comprehensive laboratory, pharmacy, clinical diagnosis and treatment rooms, infusion space, a delivery suite, capacity for wet and dry storage, and safe medical waste incineration and disposal. Community health workers constitute mobile teams providing outreach, triage, treatment and follow-up services to a geographically dispersed population. All medical care is provided free-of-charge." Nyaya Health, "Overview."
- 3
Nyaya Health, "Budget."
- 4
Data from Nyaya Health, "Nyaya Health Budget," Sheet Budget Input. Data analysis in GiveWell, "Nyaya Health Expenses (2010)," Sheet Analysis.
- 5
Data from Nyaya Health, "GiveWell HMIS Summary."
"We unfortunately do not have any old General/Outpatient Registers prior to Magh 2066 [January/February 2010], nor do we have any record of the HMIS summary reports from that time." Nyaya Health, "GiveWell HMIS Summary." Nyaya Health does present numbers of emergency patients and abortions performed starting in June 2009, when the hospital opened, but for consistency only tallies starting January 15, 2010 are presented here. See Nyaya Health, "Nyaya Health opens Bayalpata Hospital in Achham" for date of hospital opening. - 6
Nyaya Health, "Developing an X-ray Program in Achham."
- 7
Nyaya Health, "ART Enrollment by Month."
- 8
Nyaya sent data for the two months February 15 to April 15, 2011, the Nepali months of Falgun and Chaitra, the first of which includes outpatient diagnosis, and the second of which includes diagnosis for outpatients, emergency patients, and inpatients. Nyaya initiated a new data collection system starting February 2011, and we do not know whether this data was being collected prior to that. There is diagnosis data from an earlier period, 2008-2009, on Nyaya'a website (see Nyaya Health, "Outpatient Data"), but we haven't seen it for the intervening period. Below we have reproduced data from the March 15 to April 15 report, which is the only report we have seen that includes diagnosis from outpatients, inpatients, and emergency patients (from Nyaya Health, "Calculations for Chaitra 2067," Sheets NH OPD ICD, NH Emergency ICD, and NH IPD ICD.) Note that the data may contain some errors: "You will see that there are still inconsistencies / discrepancies in some of our automatically generated data, as compared to the hand-recorded data, which is a result of several data entry problems some of which are due to user-entry error and some of which are due to our own inability (thus far) to account for complicated data algorithms, for example avoiding duplicate or triplicate counting when one patient has more than one diagnosis." Dan Schwarz, email to GiveWell, May 5, 2011.
10 most common outpatient diagnoses:- Gastritis (APD): 432 patients
- Upper respiratory tract infection: 289 patients
- Other Musculoskeletal/Rheumatic: 148 patients
- Headache: 105 patients
- Urinary Tract Infection (UTI): 91 patients
- Menstrual disorder: 74 patients
- Intestinal worms: 68 patients
- Fall/Injury/Other Trauma: 65 patients
- Eczema/Dermatitis: 64 patients
- Back pain: 63 patients
5 most common emergency patient diagnoses:
- Gastritis (APD): 24 patients
- Fall/Injury/Other Trauma: 20 patients
- COPD: 13 patients
- Acute gastro enteritis: 9 patients
- Other Obstetrical Conditions: 9 patients
5 most common inpatient diagnoses:
- Gastritis (APD): 10 patients
- Pneumonia: 8 patients
- Fall/Injury/Other Trauma: 7 patients
- Other Obstetrical Conditions: 5 patients
- Urinary Tract Infection (UTI): 4 patients; Acute gastro enteritis: 4 patients
- 9
"The ambulance is used both to pick patients up from surrounding communities as well as to transport patients from Bayalpata Hospital to other facilities for higher-level care...360 patients = the total number of patients provided services." Nyaya Health, "Report of Ambulance Services at Bayalpata Hospital," Pgs 2-3.
- 10
Nyaya Health, "Personnel."
- 11
Nyaya Health, "Comments on GiveWell Draft Review of Nyaya Health."
- 12
Examples from Nyaya Health, "Personnel":
- "Dr. Bikash Gauchan: Dr. Gauchan grew up in the village of Kalopani in Lete VDC of Mustang district of Nepal. He attended the Gyanodaya Secondary School and ED- Mark Academy Higher Secondary School. He then attended medical school at B.P. Koirala Institute Of Health Sciences(BPKIHS) in Dharan. Following graduation Dr. Gauchan worked at BPKIHS for one year, initially as a House Officer in the department of General Practice and Emergency Medicine and later in the department of Anesthesiology and Critical Care."
- "Drona Awasthi: Mr. Awasthi completed his Lab Assistant degree from CICD Campus, Dhangadi. Before joining Nyaya, he worked at Sewa Nursing Home, Attariya. His arrival at Nyaya has nearly doubled the capacity of the free Diagnostic Laboratory, allowing the lab to meet the increasing patient load in Achham. Mr. Awasthi works to conduct quality control of the lab services and has received several trainings to supplement his academic coursework, enabling him to operate the state-of-the art equipment that have been purchased by Nyaya or donated from institutions in the US. Mr. Awasthi is from Kailali, a twelve hour bus ride from Sanfebagar."
- "Urmila Basnet: Ms. Basnet was born in Jajarkot district and moved to Sanfebagar after her marriage. She brings extensive experience in midwifery and family planning to Nyaya. She worked as a midwife distributing contraceptives and providing counseling for one year for the Dhankuta District Family Planning Association. Following that, she spent five years with Paryojana, an NGO promoting family planning in Achham. Her work focused on pregnant women and involved traveling to remote areas to dispense medications, immunizations and advice on family planning. After that Ms. Basnet spent one year providing care to HIV-positive patients for an HIV/AIDS service organization in Achham. Ms. Basnet, along with the rest of the team of midwives, operate the free 24-hour birthing center at the Bayalpata Hospital, conduct free antenatal care and counseling, and assist in triage and patient flow at the Outpatient Department."
- 13
Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham," Pg 1.
The report from this survey implies that at that time (2007), access to public medical facilities was poor - specifically:
- The district hospital was accessible only via an unpaved road, and its eight inpatient beds were "usually full."
- "District Hospital in Mangalsen: This is the main referral center for the district of 250,000 people. It is highly inaccessible, however, given that the roads to it are unpaved. The road from Sanfe is slowly going to be making its way to Mangalsen, to be completed perhaps in 3 years. About 40 staff run both the hospital and district public health office, which is located in the hospital. Currently, the hospital and public health program is headed by the DHO, an MBBS doctor about 12 years experience, including public health experience. Laboratory and diagnostic capabilities include AFB smear, X-Ray, hemoglobin, manual CBC, glucose, HIV, bilirubin, gram stain, blood smear, urine and stool microscopy. They perform vacuum-assisted deliveries, manual removal of placenta, incision and drainage, suturing of lacerations, and external reduction and casting, but do not do c-sections or any other surgeries, blood transfusions, thoracentesis, or paracentesis. It has an inpatient unit with 8 beds, and is typically full. An operation theatre is being constructed by the German development agency GTZ and will be completed in 4 months." Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham."
- Of the 58 households surveyed, only one reported having used the district hospital in the previous year (while 11 reported having traveled to India for medical care and 2 to Katmandu).
- "The survey questionnaires were administered to 58 households...Eleven (19%) of households had made at least one trip in the last year to India for medical care, and an additional two (3) had made the (typically longer) journey to Kathmandu...Only one household reported the use of the Mangalsen district hospital in the past year." Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham," Pgs 2 and 5.
- The nearest surgical center was 8 hours away by bus, and the nearest hospital with antiretroviral treatment for HIV/AIDS was 3.5-4 hours away by bus.
- "TEAM hospital in Dadeldura (about 8 hours away and 300-400 Rs. by bus). This mission hospital is the closest provider of surgical (including c-section) and transfusion services." Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham."
- "ARVs remain available only in the Doti district hospital, which for most of the communities is 4-5 hours away. One survey of migrants returning from Bombay found 8% of those tested to be seropositive for HIV. This survey was carried out six years ago, and more recent data is not available." Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham." The same report says, "Outside of Achham, individuals can access services at the Doti District Hospital about 3.5 hours by bus from Sanfe (about 150 Rs)."
- Another NGO was working on expanding the capacity of the district hospital, and the road was also being paved; it's our understanding that the paving is not yet complete but that the government is aiming for completion in 2011.
- "GiveWell: You mentioned that government services have changed since you got started. What has changed and why?
Nyaya Health: To give you a very brief history of Nepal, there was a civil war that started in 1996, and, depending on who you ask, ended in 2006 (some would argue that it's still going on), between the government and the Maoist rebels. Maoists were centered in the general region where we are. In addition to being decimated during the war, it also suffered political marginalization and virtually lack of any development or investment...Since 2006, the peace accords were signed. There has been a slow rise in increased investment in the area. It's in the government's strategic benefit to invest in the area. It's received more development than it had previously...
GiveWell: How would you respond to the possibility that health would have gotten better without Nyaya's involvement?
Nyaya Health: Things would have gotten better and have gotten better outside of what we've done. I do think that Nyaya's presence has had a very positive impact on the support Achham has been offered. Our contract with government alone is an infusion of almost $50,000 per year that otherwise would have not have been there. Other districts in the region have not received the same investment because they don't have an NGO that the government is partnering with...
GiveWell: What are the additional government investments (outside of Nyaya's contract)?
Nyaya Health: I'm not sure how specific I can get. I know that the district hospital in Mangalsen has a few more employees. There are two doctors. They have some additional equipment. Hypothetically, their supply chain and medication stocks are a bit better. It's hard for me to say with confidence. Our impressions of the local health post is very varied. Some are at least as bad as when we got there, some marginally improved. The per capita expenditure on health is $5 per capita in 2007. I know it's increased, but I don't know by how much.
GiveWell: Has the road to the district hospital been completed?
Nyaya Health: No, road has not been completed. It was extended 2-3 miles in 2010. It's still another 5-10 miles away from the district hospital. I'm really not sure. It's supposed to be done in 2011, but it remains to be seen...
The doctor who does c-sections at the district hospital is only there every couple of weeks." Ryan Schwarz, phone conversation with GiveWell, March 31, 2011. - One of the M&M reports (discussed below), from August 2010, says, "Bajura is far from our hospital. There is no paved road all the way to Bajura. There is district hospital but doctor is not available all the time." Nyaya Health, "M&M Review (August 25, 2010)."
- "GiveWell: You mentioned that government services have changed since you got started. What has changed and why?
- The condition of health centers and health posts was extremely poor. There were two "minimally functioning" and inaccessible primary health centers without doctors.
- "Primary health centers (PHC). PHCs should be staffed by at least a doctor and be capable of running basic laboratory tests. There are two of these in all of Achham, but they are less accessible to the Sanfe Bagar communities than even the district hospital. According to the DHO, these are minimally functioning. Neither have a doctor. We did not visit these given their large distance from our catchement area." Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham."
- Health posts that were staffed part of the time and had expired medicines.
- "Healthposts/sub-healthposts. These ideally would function as triage services run by the AHWs, HAs, and ANMs. We have not found a single one in the area that is functional beyond serving as relay stations for vaccination programs and distribution of some basic medicines. We visited the Masta Mandu, Hatikot, Siddeswor, Ridikot, and Jaypaldevi sub-healthposts, and there was little variation between them. They were typically staffed by an AHW or CMA, an ANM, a VHW, and a peon. The norm is that the government healthworkers operate private practices, and most posts have expired medicines; the medicines come once a year and within a few months the supply has ceased. The Badalgada hospital is functioning technically as a healthpost and is worth mentioning because it was originally the site that the Ministry desired Nyaya to renovate and staff. It operates a few days a week with staff of a CMA, an ANM, and a peon. Both the CMA and ANM have private practices that are more of a priority. The maintenance was very poor, and again had an old stock of expired medicines." Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham."
- The main source of health care was private, and the level of wealth in the area was extremely low.
- "As is typical for most of South Asia, 80-90% of healthcare activities are done by private medical practitioners. Most of that other 10% consists of vaccines, TB, and occasional health camps. There is typically one private 'medical' (clinic) in each village, although Sanfe has five. The privates often work or have worked in the government as low-level practitioners (auxiliary health workers, health assistants, auxiliary nurse midwives)." Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham."
- "Achham district in Far Western Nepal is home to 250,000 people and is extremely poor and undeveloped even compared with the national averages. Annual income averages $141, while 92-95% of homes don’t have electricity and the average level of education is 1-1.5 years of schooling. A staggering 60% of children are malnourished. Labor migration rates are among the highest in the country, with 40-90% of households having a member working seasonally in India. Not coincidental to these circumstances, this district is believed to have one of the highest rates of HIV in Nepal. Development in Achham has been slow to progress, despite urban economic growth and health progress. The average income in Kathmandu is 4.5 times that of Achham and grew, in terms of purchasing power parity, more than $300 dollars between 1996 and 2001, while dropping $7 in Achham. Likewise, while the national literacy level rose 12% over this period, it only rose 1% in Achham, to 26%. Fifty-five percent of the population in Achham doesn’t have access to safe drinking water, two and a half times the national average." Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham," Pgs 2-4.
- "The median monthly household income was 2000 Rs (30$US), or about 70 Rs. ($1) per day. The national population survey of 2001 reported an annual per capita income in Achham of $141, translating into approximately $0.40 per day. The median ropanis per household was 3, and each ropani produces approximately from 5,000-10,000 Rs. per year." Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham," Pg 3.
- For the 11 households (of the 58 surveyed) who had made at least one trip in the last year to India for medical care, "the median amount spent (Rs 11,500) is equivalent to nearly 6 months of the median household income."
- "Eleven (19%) of households had made at least one trip in the last year to India for medical care, and an additional two (3) had made the (typically longer) journey to Kathmandu. These trips last over one day of solid travel one-way, for medical services. The costs of these medical journeys were 510, 2500, 3000, 4000, 11000, 12000, 20000, 22000, 25000, 35000 Rs (two were not recorded). The median amount spent (Rs 11,500) is equivalent to nearly 6 months of the median household income. Only one household reported the use of the Mangalsen district hospital in the past year." Nyaya Health, "Health Services Assessment in Five Village Development Committee Areas Surrounding Sanfe Bagar, Achham."
- The district hospital was accessible only via an unpaved road, and its eight inpatient beds were "usually full."
- 14
- "The Nepali Civil War (labelled People's War by the Maoists) was a conflict between government forces and Maoist rebels in Nepal which lasted from 1996 until 2006." Wikipedia, "Nepalese Civil War."
- "The area we work in is the poorest area of Nepal was the epicenter of the civil war. It is where the rebel Maoists had their base. The government systematically destroyed everything over 10 years of fighting the rebels." Ryan Schwarz, phone conversation with GiveWell, February 17, 2011.
- 15
"I know that the district hospital in Mangalsen has a few more employees. There are two doctors where previously there weren't any. They have some additional equipment. Hypothetically, their supply chain and medication stocks are a bit better. It's hard for me to say with confidence." Ryan Schwarz, phone conversation with GiveWell, March 31, 2011.
- 16
"In terms of investments however, as Nyaya has increased infrastructure (a health center, a hospital, a CHW network) in the region, we have provided further opportunity for government investment than previously existed. Ministry HR policy allocates staff per facility and therefore gross numbers of facilities drives number of staff funded for each district. As the table below demonstrates, there are now 4 MBBS physicians in Achham, 2 of whom are at the Ministry district hospital, and 2 of whom are supported by the Ministry to work at our hospital. Neighboring districts, Bajura and Doti - similar in size, population, geographic isolation and development indices to Achham - during the same time period, also saw an increase in number of physicians. However, as each district has only one hospital, they have necessarily received fewer staff." Nyaya Health, "Nyaya Health’s Impact in Public-Sector Strengthening: Addressing the Counter-Factual Hypothesis."
- 17
GiveWell: What is the schedule of visits by non-staff medical professional to the hospital, i.e. how often are observers there?
Nyaya Health: Our Executive Director is an ex-pat who lives there and that's a critical communication link for us. People go out there pretty regularly. We have a reasonable constant ex-pat presence, and when I say ex-pat, I also include Nepalis who are part of the Nepali diaspora in the US. The value added of someone like Michael Polifka is huge. The staff loved him. His biggest impact comes from modeling professionalism.
We normally have 1 or 2 out there at all times, though it's not part of our model. They're not there to provide direct medical care, but they're there to train. They're only there for a few weeks, but they have an impact on knowledge dissemination."
Duncan Maru, phone conversation with GiveWell, March 17, 2011. - 18
Michael Polifka, phone conversation with GiveWell, March 14, 2011.
- 19
She continued, "Most government health facilities have very high rates of staff absenteeism. What you'll find is that the doctor might be present for 1-2 months of the year at the district hospitals. Having doctors on-site and providing continuity of services are key quality indicators. Nyaya Health provides continuous services and has 2 doctors on site for 12 months of the year...
In a case we had last night a middle-aged woman who was grazing her animals was about to tie up her bull when it attacked her...Dr. Amir cleaned the wound, controlled the bleeding, provided IV and local pain meds, and did an excellent job of suturing the muscle and skin. She's now doing well as an inpatient. If this hospital weren't here, she would have had to travel another 6 hours (by jeep)....The hospital is good at handling cases of severe pneumonia in children under 5. These cases are excellently managed with IV antibiotics, inhalers, and oxygen as needed...People have started hearing about the hospital and the free care, and have started to come after other facilities were unable to solve their problems.
One of the main things that is not handled well is pain control...Doctors are hesitant to use morphine for example. We recently had a case of acute heart failure where I would have thought first about morphine, but that's not how the doctor handled it...Most of the time it's not so much that a case was badly managed but that the staff don't have the tools to make a diagnosis." Ruma Rajbhandari, phone conversation with GiveWell, March 18, 2011.
Dr. Rajbhandari also wrote on the Nyaya Health blog about two traffic accidents that the Bayalpata Hospital staff responded to while she was there. She identified both strengths and weakness in the way the cases were handled: "The teamwork among the staff in dealing with a disaster such as this was absolutely remarkable. I smiled as our Hospital Administrator went around making sure that everyone had gotten their Tetanus booster shots...That’s not to say there weren’t problems. There were many things that could have gone better. Infection control in our procedure room needs to be improved. Many of our suture kits do not have the proper instruments. We lack certain supplies like face shields, booties and sufficient gowns to protect our doctors and nurses from coming into contact with bodily fluids. We also did not have sufficient staffing to deal with a disaster such as this and attend to the one-hundred or so OPD patients that had walked many hours to see a doctor that day." Nyaya Health, "'We can only take the severely injured right now…'"
- 20
Nyaya Health, "Norwegian Group Visit to Bayalpata Hospital."
- 21
She continued, "I have been very impressed with the dedication, volunteerism of almost everyone involved with Nyaya who work hard under difficult conditions to bring quality health care to the people of Achham." She does not discuss observing patient care. Nyaya Health, "Interview with Nyaya Donor Dr. Prativa Pandey of CIWEC Clinic."
- 22
He continued: "The illnesses that come through the door are amazing: many people with active TB; a 16-year-old with severe rheumatic heart disease; women with traumatized pelvic organs from a traditional healer placing a stick in the uterus and leaving it there to produce sterility or induce an abortion. There are many fractures of arms, legs, and wounds that resist healing. The inpatient ward is mostly women with severe end stage emphysema from breathing smoke during cooking." Lichtenstein and West 2011.
- 23
Ryan Schwartz, phone conversation with GiveWell, March 31, 2011.
- 24
The following is from Nyaya Health, "Cases."
Overview of case Date of report Problems identified Report Fetal demise in 20-year-old July 22, 2010 Low supplies, lack of staff training, difficulty of travel Nyaya Health, "Mortality Report: Intrauterine Fetal Demise in a 20yo Primagravid (July 22, 2010)." 19-year-old woman came in a few days after childbirth with fever and was transferred July 28, 2010 Absence of lab assistant, disorganization of emergency area, lack of follow up after delivery, dosing guidelines, electrical infrastructure, and staff organization Nyaya Health, "Mortality Review: 19 Year Old Woman with Retained Products of Conception (July 28, 2010)." Two young brothers died of poisoning August 4, 2010 Lack of protocols for emergency care, equipment in inconvenient location, lack of advanced equipment, inconvenient location of electrical outlets, and lack of staff training. Nyaya Health, ""MMC: 12 and 6 Year Old Brothers Dead of Unknown Poisoning (July 27, 2010)." 28-year-old male attempted suicide August 10, 2010 Some medicines not on pharmacy list, lack of psychiatrist in the area Nyaya Health, "Morbidity review: Suicide attempt by 28 year-old male (August 10, 2010)." 87-year-old male died after 6 weeks in the hospital he was transferred to August 18, 2010 Low stock of one medicine due to supply chain issues Nyaya Health, "Mortality Review: COPD." 35-year-old female with prolonged labor and stillbirth August 25, 2010 Lack of some laboratory services, and lack of training for some staff in forcep and vacuum delivery and for CHWs in danger signs. Nyaya Health, "M&M Review (August 25, 2010)." 8-month-old infant died at hospital September 6, 2010 No electricity, disorganization, lack of staff skills and intensive care Nyaya Health, "Mortality Review: Septic Shock (September 6, 2010)." Adult female victim of a road traffic accident died at hospital September 17, 2010 No electricity and lack of x-ray, ECG, and certain supplies Nyaya Health, "Mortality Review: Motor Vehicle Death (September 17, 2010)." 22-year-old female required manual removal of her placenta September 30, 2010 Equipment malfunction Nyaya Health, "Manual Placenta Removal (September 30, 2010)." 17-year-old girl died of parasitic disease October 11, 2010 Lack of needed testing materials, blood transfusion capacity, and funding for further care Nyaya Health, "Mortality Review: Kala-azar (October 11, 2010)." 25-year-old female stable after procedure for incomplete abortion November 5, 2010 Limited laboratory capacity Nyaya Health, "Molar Pregnancy vs. Incomplete Abortion (November 5, 2011)." 30-year-old female came in with an infected abortion and was transferred for surgery January 17, 2011 Lack of staff training Nyaya Health, "M&M: 30 y/o Infected Abortion (January 17, 2011)." 60 year-old male diagnosed and treated for TB January 24, 2011 Staff away, not enough time for seeing outpatients, disorganization, lack of some equipment, miscommunication Nyaya Health, "M&M: 60 y/o male with TB (January 24, 2011)." 11-month-old female died of malnutrition and diarrhea January 31, 2011 Lack of supplies and community awareness. Nyaya Health, "Mortality Reivew: 11 Month Old with Severe Acute Malnutrition and Diarrhea (January 31, 2011)." 17-year-old male brought dead after a fall February 5, 2011 Expired medicines, emergency materials unorganized, too few beds, delay in calling the ambulance, and poor roads. Nyaya Health, "Mortality Review: 17yo Male with Head Trauma (February 7, 2011)." 65-year-old male with suspected liver failure February 15, 2011 Broken or missing supplies, ambulance unavailable Nyaya Health, "Mortality Review: 65yo COPD with Suspected Liver Failure (February 14, 2011)." - 25
"In Katmandu, there's no shortage of healthcare and there are plenty of doctors and surgeons. Convincing those doctors to come to rural areas – where there aren't good schools for their children, for example – is difficult. The hope is that by developing more infrastructure capacity in rural areas, we shift surgeons from urban areas to rural ones." Ryan Schwarz, phone conversation with GiveWell, February 17, 2011.
- 26
Ryan Schwarz, email to GiveWell, March 14, 2011.
- 27
"GiveWell: How would you respond to the possibility that health would have gotten better without Nyaya's involvement?
Nyaya Health: Things would have gotten better and have gotten better outside of what we've done. I do think that Nyaya's presence has had a very positive impact on the support Achham has been offered. Our contract with government alone is an infusion of almost $50,000 per year that otherwise would have not have been there. Other districts in the region have not received the same investment because they don't have an NGO that the government is partnering with." Ryan Schwarz, phone conversation with GiveWell, March 31, 2011. - 28
For example, Nyaya Health, "Financial Statements (2009)," Pg 2 show that Nyaya Health received $22,500 from the Nepal government in that year.
- 29
"Government funding has historically been centered in the eastern and central regions of Nepal." Ryan Schwarz, email to GiveWell, March 14, 2011.
Chin, Montana, and Basagña 2011 present data suggesting that health care access and health outcomes (pre-2006) were worse in the Far Western region in which Nyaya works than in the eastern and central regions. - 30
Nyaya Health, "Nyaya Health’s Impact in Public-Sector Strengthening: Addressing the Counter-Factual Hypothesis."
- 31
Ryan Schwarz, email to GiveWell, March 14, 2011.
- 32
Ryan Schwarz, email to GiveWell, March 14, 2010.
- 33
Nyaya Health stated (above) that it had raised about 35% of $400,000 (i.e. about $140,000) between the start of the year and mid-March 2011. On June 8, 2011, Nyaya Health announced that it had raised $175,000 since April 1, 2011: "On April 1st, The Nick Simons Foundation generously donated $25,000 to Nyaya and offered an additional matching donation of $75,000 more – the total donation, if Nyaya was able to raise $75,000 ourselves, would equal $175,000! I write today to announce that with your support Nyaya has not only reached that goal, but done so in record time! While we had set what we thought was an overly ambitious deadline of July 1st, 2011, to raise the $75,000, with your commitment to this work we were able to raise the money in only 2 months!" Nyaya Health, "Nyaya raises $75,000 to be matched by Nick Simons Foundation in 2 months!"
- 34
Nyaya Health, "Budget." See heading "Current Account Balances."
- 35
Nyaya Health, "Differential Funding Scenarios (2011)."
- 36
Nyaya Health, "Expansion Costing."
- 37
From Nyaya Health, "Expansion Costing," Sheet Demography:
Minor Surgery, >15 years old: 30 minutes
Major Surgery, >15 years old: 100 minutes
Minor Surgery,15 years old: 50 minutes
Major Surgery, 15 years old: 130 minutes
Orthopedic surgery, non-trauma: 100 minutes
Cesarean Section: 50 minutes
Trauma/Accident: 80 minutes - 38
This is likely to be an underestimate as it assumes that the proportion of total spending on community health in 2010 was the same proportion of total spending in 2011. We have estimated it this way because we do not have a figure for the cost of the community health program in 2010. However, it is our understanding that the community health program is a key priority of Nyaya Health's and, therefore, is likely being scaled up at a faster rate in 2011 than other programs (surgical and transfusion excluded).
- 39
GiveWell, "Nyaya Health Funding Gap Analysis."
- 40
Nyaya Health, "Expansion Costing," Sheet Operating. Note that the meanings of the acronyms VDC and FCHV were checked by searching Nyaya's blog for those terms.
- 41
GiveWell, "Nyaya Health Funding Gap Analysis."
- 42
GiveWell, "Nyaya Funding Gap Analysis" and Nyaya Health, "Expansion Costing," Sheet Operating. Note that we have included the costs labeled "FCHV Program Costs: Achham" in Community Health rather than General as it is in the planning document.
- 43
GiveWell, "Nyaya Health Funding Gap Analysis."
- 44
Nyaya Health, "Expansion Costing," Sheet Operating. Note that an exchange rate of 72 NRs. per USD was used as indicated in Nyaya Health, "Expansion Costing," Sheet Demography.
- 45
Nyaya Health's expenses in 2010 were $162,494. Subtracting this amount from what (we estimate) has been raised in the first half of 2011, leaves a surplus of $152,506 to be used toward expansion. Subtracting $152,506 from the total budget for expansion ($1,073,026) leaves $920,520 to be raised.
Note that this analysis assumes that (a) Nyaya can expect to maintain funding from current sources at its 2010 level in 2011-2013; and (b) that sources of additional funding in 2011 are not expected to be renewed. We consider these to be reasonable assumptions given the information we have. They have not been confirmed by Nyaya Health.
- 46
"We know in the development field that the development of primary health care structures is very important for enhancing health across the population. We're the only facility doing it and the only facility doing it for free...The government hospital does charge for all of its services. The user fees there are a significant barrier...We are working with the government and we want to show the government that more people show up when you don't charge." Ryan Schwarz, phone conversation with GiveWell, March 24, 2011.
- 47
"Since January 2009, under the "New Nepal, Healthy Nepal" initiative of the Government, all citizens are able to access District Hospitals (DH) and Primary Health Care Centres (PHCC) without having to pay for registration: they are eligible for free outpatient, emergency and in-patient services, as well as drugs. A second universal programme commenced in January 2008, aimed at the provision of free essential health care services to all citizens, whether poor or not, at Health Posts (HP) and Sub-Health Posts (SHP) nationwide. There are no charges for registration or for the dispensation of 32 essential drugs at the HP level and of 22 drugs at the SHP level...Utilization increased substantially after the policy was implemented." Though the report also notes, "At present, there are shortages of doctors and of hospital beds...There were drug stock-outs in 29 percent of the cases...Many people remain unable to reach a health facility because of distance, cost of transport, and, for some, lack of knowledge that services are free of charge. Waiting times at facilities and poor quality of treatment at facilities may also remain as barriers for disadvantaged groups...Budget for free care [is] unlikely to meet full needs." GTZ, "Free Health Care in Nepal: Findings of a Rapid Assessment."
